Help broken ribs heal faster – how to know if you re healing normally
Yes, there are surgical interventions for rib fractures. These may depend on your situation and if the injury is in conjunction with other issues like nerve or muscle damage. A doctor will often take a look inside the chest cavity to ensure the lung is not trapped in the fracture as that can cause ongoing pain. The diaphragm is also examined to make sure there is no injury to it. “If you’ve received a diagnosis of slipping rib syndrome, it can be surgically corrected as well. An operative option includes reducing the rib fractures and placing a titanium plate across the fracture. These plates can be placed on the inside of the rib or the outside, depending on their location. The plates are held in place with titanium screws. This allows for better chest wall stability and allows the fracture ends to realign to expedite healing,” says Dr. Bauman. “We also perform cryoablation of the intercostal nerves of each rib. This stuns the nerve causing it to become numb for about three to six months, but the nerves eventually return to normal as the ribs heal. This treatment can significantly help with rib fracture pain.”
How Are Broken Ribs Treated?
Unlike other types of bone fractures, broken ribs aren’t treatable with a cast or splint. They usually are treated without surgery but on occasion surgery is required.
For a long time, broken ribs were treated by wrapping the torso tightly. But experts have since found that this isn’t very helpful. Plus, it made it hard to breathe deeply, which is important for reducing your risk of pneumonia or other respiratory complications.
Today, treatment for broken ribs typically focuses on a combination of rest, pain management, and breathing exercises.
Indications for surgical intervention include a flail chest (three or more adjacent ribs broken in multiple places) or multiple rib fractures that are causing breathing problems.
If you’ve broken a rib (or several), one of the best things you can do is simply rest. This will not only reduce some of the pain but also help your body navigate the healing process.
Still, you need some level of physical activity for the rest of your body and overall health. You’ll be able to get up and walk around pretty early in the recovery process, but it’s best to wait until your healthcare provider gives you the green light.
Once you get the go-ahead to start walking around, you can also return to other low-impact activities, including:
- sexual activity
- light housework
- simple errands
- working, as long as it doesn’t involve heavy lifting or physical exertion
Things to avoid
As you recover, there are certain things you shouldn’t do, including:
- lifting anything over 10 pounds
- playing contact sports
- doing any activities that require pushing, pulling, or stretching, including crunches and pull-ups
- engaging in high-impact activities, such as running, horseback riding, or ATV riding
- playing golf; even that gentle swinging can cause excruciating pain if you have a broken rib
The main symptom of broken ribs is ongoing pain, so controlling that pain and discomfort is essential to a better recovery. Reducing your pain, even a little, can allow you to breathe normally and cough without too much discomfort.
Prescription medication
Initially, you’ll probably be prescribed prescription pain medication to help you get though the first few days. Common examples include oxycodone (Oxycontin) and hydrocodone (Vicodin).
Warning
Oxycodone and hydrocodone are strong opioids that carry a high risk of addiction. Only take these medications as directed.
Avoid driving while under the influence of opioids. Also avoid drinking alcohol.
Talk to your doctor about medicines you’re already taking if they prescribe opioids to you for pain. Some medications, such as sleep aids and anti-anxiety medications, should not be taken simultaneously with opioids.
Over-the-counter (OTC) medication
After you get past the initial pain, you’ll want to start swapping prescription medication for an OTC option. Nonsteroidal anti-inflammatory drugs, such as ibuprofen (Advil) or naproxen (Aleve), should do the trick.
You can also holding a covered icepack against the area for 20 minutes at a time three times a day for extra relief.
Pain that lingers or gets worse for more than three weeks or so should be reported to your doctor.
Taking big, deep breaths causes your lungs, which are protected by your ribcage, to expand. Usually, this isn’t a problem. But if you have a broken rib, taking a deep breath can be painful.
Taking only shallow breathes can increase your risk of developing pneumonia and other respiratory illnesses. This is why you’ll likely be sent home with some breathing exercises to do as you recover.
You may even be advised to work with a respiratory therapist. Part of your therapy may include the use of a spirometer, which is a device that measures the volume of air you breathe in and out. This will give you a better idea of how it should feel to take a full, deep breath.
To help with the pain, consider taking your pain medication just before you start your breathing exercises. Holding a pillow gently, but firmly, against your chest may lessen the pain. Work on just taking slow, steady, deep breaths.
Try this
Here’s a quick breathing exercise to add to your recovery plan:
- Start with three seconds of deep breathing.
- Switch to three seconds of relaxed breathing.
- Do a few “huffs” or short breaths with some light coughs.
- Finish off with another three seconds of relaxed breathing.
- Repeat this cycle several times.
Each rib injury and recovery period is unique, but in general, broken ribs take about six weeks to heal. That time frame could be shorter if the fracture is mild.
If internal organs, such as your lungs, were also injured, a full recovery could take longer. This is especially true if you needed surgery to repair the damage.
Occasionally, rib injuries can cause damage to your lungs. Usually, any lung damage will be diagnosed during your initial exam. But sometimes, lung injuries aren’t noticeable right away.
As you recover, you’ll want to keep an eye out for any signs of a punctured lung or pneumonia.
Seek immediate medical care if you experience:
- difficulty catching your breath
- coughing up mucus more often or coughing up thicker mucus
- coughing up blood
- blue lips
- fever of 102ºF (38.8°C) or higher
Most cases of broken ribs resolve without surgery. But you’ll need to make sure you give your body plenty of rest while keeping your lungs in good working order. You should be back to most of your usual activities in a month or two.
If you find that the pain, even with prescription medication, is too much, don’t hesitate to talk with your doctor about your options. A nerve block for pain may be helpful, especially at first.
Last medically reviewed on January 28, 2019
Help broken ribs heal faster – how to know if you’re healing normally
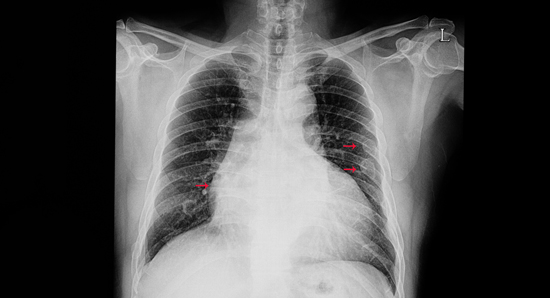
Have you injured yourself and suspect a fractured rib? Perhaps you even went to the emergency room, found out you have a few broken ribs and went home waiting for them to heal over time. What should the healing process look like? How do you know if the pain has been going on for too long? Here’s some advice.
How long does it take for rib fractures to heal?
Rib fractures take a little longer to heal than other bones because they are continuously moving. A rib fracture can take up to 12 weeks to heal. “The natural progression for healing is for small improvements in pain and breathing over time. For patients with rib fractures without fixation (surgical stabilization of rib fractures), roughly 60% are not back to full work capacity at six months, and 70% are still having some degree of pain one year from the injury,” says Zachary Bauman, DO, Nebraska Medicine trauma medical director.
What can I do about the rib pain?
Typically, nonoperative treatment includes a pain medication regimen such as:
- Scheduled acetaminophen with a combination of ibuprofen as needed
- Neuropathic pain medications (target nerves specifically)
- Lidocaine patches
- Prescribed muscle relaxants and narcotics
- We always encourage aggressive pulmonary hygiene with deep breathing and coughing to help with volume expansion
How do I know if the pain has gone on too long?
A good percentage of rib fractures will heal on their own, especially if the ribs are in alignment. For ongoing pain that doesn’t seem to be improving, persistent shortness of breath with activities you didn’t previously have shortness of breath, or if you haven’t returned to normal daily activities after several months, it may be time to seek additional medical help. If you’re feeling ongoing clicking, popping, or movement at the fracture site – even if it comes and goes with various activities – see a doctor for further evaluation.
Are there surgical options for broken ribs that don’t heal?
Yes, there are surgical interventions for rib fractures. These may depend on your situation and if the injury is in conjunction with other issues like nerve or muscle damage. A doctor will often take a look inside the chest cavity to ensure the lung is not trapped in the fracture as that can cause ongoing pain. The diaphragm is also examined to make sure there is no injury to it. “If you’ve received a diagnosis of slipping rib syndrome, it can be surgically corrected as well. An operative option includes reducing the rib fractures and placing a titanium plate across the fracture. These plates can be placed on the inside of the rib or the outside, depending on their location. The plates are held in place with titanium screws. This allows for better chest wall stability and allows the fracture ends to realign to expedite healing,” says Dr. Bauman. “We also perform cryoablation of the intercostal nerves of each rib. This stuns the nerve causing it to become numb for about three to six months, but the nerves eventually return to normal as the ribs heal. This treatment can significantly help with rib fracture pain.”
As a nationally certified Level I trauma center, the Nebraska Medical Center provides the highest level of care for the most severe and life-threatening injuries for both children and adults. If you are experiencing symptoms or your pain hasn’t resolved over time, we are here to help.
To set up an appointment for evaluation of a suspected rib injury, please call 402.559.6075.
Related stories:

Innovative rib surgeries lead to speedier recovery after traumatic car accident
Nebraska Medicine surgeons are now offering rib and sternal fracture surgery that is speeding up recovery from chest wall injuries by increasing mobility, reducing pain and use of narcotics and lowering mortality.

Trauma center helps young family recover from horrific car accident
The Nebraska Medical Center Level 1 trauma center has a comprehensive availability of resources to provide an entire spectrum of care any time of the day or night to address the needs of children and adults. Learn how the trauma center helped one young family survive a horrific head on car accident.
6 Steps for Healing Broken Bone (Fractures) Faster
4. Boost your mineral intake to include all 20 key bone building nutrients.
5. Enhance vitamin intake
6. Avoid Smoking & Alcohol
Those of us who have experienced a significant fracture likely recall first the pain of the injury, then we often focus our attention on the prospect of time in a cast or other form of extended immobilization during the fracture healing process. We imagine the discomfort and limitations that will ensue, and after all else settles down, we often wonder, “How strong are my bones anyway, and will I fracture again?”
Nature, on the other hand, has no such questions, but moves swiftly to initiate healing. Guided by a complex intelligence that we do not yet fully understand, bone repairs itself — and over a few months is made whole again. The fracture self-repair process is spontaneous, natural, and seeks no direction from us, but what we do during this time is of unrecognized importance. The stage we set for healing greatly influences the speed, comfort, and completeness of the bone renewal process. Further, life-supporting changes made in response to a fracture can strengthen our entire skeleton and reduce the likelihood of future fractures.
Physiology of fracture healing
Fracture healing involves complex processes of cell and tissue proliferation and differentiation. Many players are involved, including growth factors, inflammatory cytokines, antioxidants, bone breakdown (osteoclast) and bone-building (osteoblast) cells, hormones, amino acids, and uncounted nutrients.
Fracture healing can be divided into three phases. The inflammation phase is the first stage of healing. Immediately upon fracture, a blood clot forms, allowing the influx of inflammatory, clean-up cells to the wound area. This is followed by a cytokine cascade that brings the repair cells into the fracture gap. These cells immediately begin to differentiate into specialized cells that build new bone tissue (osteoblasts) and new cartilage (chondroblasts). Over the next few months, these cells begin the repair process, laying down new bone matrix and cartilage. At this initial stage, osteoclast cells dissolve and recycle bone debris.
The second, reparative stage begins about two weeks after the fracture occurs. In this stage, proteins produced by the osteoblasts and chondroblasts begin to consolidate into what is known as a soft callus. This soft, new bone substance eventually hardens into a hard callus as the bone weaves together over a 6- to 12-week time period.
The final step of fracture repair is known as the remodeling phase. At this stage the callus begins to mature and remodel itself. Woven bone is remodeled into stronger lamellar bone by the orchestrated action of both osteoblast bone formation cells and osteoclast bone resorption cells.
The nutritional demands of healing
Each stage of the fracture healing process brings with it increased nutritional demands. For starters, the whole process requires a great deal of energy—which is generally supplied through the intake of calories in food. Next, healing requires the synthesis of new proteins, which is dependent upon an ample supply of amino acids derived from dietary proteins. An adequate blood supply is also mandatory for fracture healing, so anything that diminishes blood flow (such as smoking or poor circulation) slows the healing process. Also, the trauma of the fracture itself creates a biochemical burst of pro-oxidants (free radicals), causing oxidative stress that can overwhelm the body’s antioxidant reserves.
5 nutritional steps to accelerate fracture healing
People who have had a fracture aren’t often told that they can do anything to make their bones heal faster — at most, they’re told to limit the use of the injured bone or limb (not easy to do if the fracture is in your spine!). But there are a number of methods you can employ to reduce your healing time:
1. Provide the body with adequate energy
Fracture healing requires more energy than you might expect. Thus, it’s appropriate to increase your caloric intake to promote healing. In traumatic fractures of the long bones, for example, there is an immediate increase in metabolic demands that can translate into a caloric demand three times that of normal. While a normally active adult may require 2,500 calories a day, a bedridden, injured patient with multiple fractures may need 6,000 calories per day! If this demand is not met, the healing process is compromised.
2. Increase your protein intake
Bone can be imagined as being somewhat like a sponge made of living protein upon which mineral crystals are embedded. By volume, roughly half of bone is comprised of protein. When a fracture occurs, the body is called upon to gather protein building blocks together to synthesize a new structural bone protein matrix. In addition, protein supplementation increases growth factors like insulin-like growth factor-1 (IGF-1), a polypeptide that exerts a positive effect on skeletal integrity, muscle strength, immune response, and bone renewal. Protein malnutrition or under-nutrition leads to a “rubbery” callus, compared to the rigid calluses of those with adequate or high protein intake. Numerous studies document the acceleration of fracture healing with even a modest 10- to 20-gram increase in protein intake. The benefits of supplemental protein are important to everyone and especially important to those with malnutrition or low baseline protein intake. In fact, among elderly hip fracture patients, poor protein status at the time of fracture predicts fracture outcome. Those with low protein status take longer to heal, and have more complications, including death.
Specific amino acids of special importance include lysine, arginine, proline, glycine, cystine, and glutamine. Lysine, for example, is known to enhance calcium absorption, increase the amount of calcium absorbed into the bone matrix, and aid in the regeneration of tissue.
3. Increase anti-inflammatory nutrients
Antioxidants repair oxidative damage. When a bone fracture occurs, a remarkable yield of free radicals is generated by the damaged tissues. In particular, this damage occurs as the tightly bound collagen strands running through the mineral phase of bone are forcefully broken. These ruptured collagen strands interact with oxygen-yielding oxygen radical metabolites. These free radicals are associated with inflammation, further breakdown of bone collagen, and excessive bone turnover. In fracture healing, increased free-radical production can overwhelm the natural anti-oxidant defense mechanisms. In such cases, antioxidants — including vitamins E and C, lycopene, and alpha-lipoic acid — have been suggested to be beneficial in suppressing the destructive effect of oxidant free radicals on whole body systems and improving fracture healing in animal models and cultured human cell lines.
Inflammation is an essential component of the healing process in bone. Although painful, it is an important part of the cleaning-up and rebuilding process. This inflammatory process involves the cyclooxygenase (COX) enzymes COX-1 and COX-2. Many of our standard non-steroidal anti-inflammatory drugs act by inhibiting the COX-1 and COX-2 enzymes—which relieves the pain, but also delays healing. On the other hand, nourishing the body to reduce inflammation naturally speeds healing. Vitamin C, bioflavonoids and flavonols such as quercitin and proanthrocydins, and omega-3 fatty acids naturally soothe the inflammatory process and speed healing.
4. Boost your mineral intake
By weight, bone is roughly 70% minerals (calcium, phosphorus, magnesium, silicon, zinc, etc.) and fracture healing requires available minerals. Most of us under-consume minerals on an everyday basis, so drawing minerals to the healing site can often involve a process of “stealing from Peter to pay Paul.” (See our 20 key bone nutrients for details on average mineral intake.)
Specific key minerals for fracture healing include the following:
- ZINC. Some 200 enzymes require zinc for their functioning. Many of these functions involve cell proliferation. Zinc supplementation aids in callus formation, enhances bone protein production, and thus stimulates fracture healing.
- COPPER. Copper aids in the formation of bone collagen and is important to the healing process. The body’s demand for both copper and zinc rises according to the severity of the trauma.
- CALCIUM and PHOSPHORUS. The main minerals in bone are calcium and phosphorus, in the form of calcium hydroxyapatite crystals. This hydroxyapatite compound plays an important role in regulating the elastic stiffness and tensile strength of bone. The building and rebuilding of bone tissue requires adequate supplies of both calcium and phosphorus, which can be supplied from diet and bone reserves. Early research suggested that fractures can heal normally independent of dietary calcium and indeed it has been found that during the first few weeks of healing, calcium is drawn from the skeleton for fracture healing. After that, the diet provides the calcium necessary for fracture repair. Calcium adequacy at the RDA level is important, but unusually high intakes do not appear to speed fracture healing. As calcium absorption is dependent on vitamin D, these nutrients work synergistically. Human studies, in fact, suggest that for best fracture healing both calcium and vitamin D should be obtained in optimum daily levels. Most of us consume plenty of phosphorus and often too much if the diet is high in processed foods and colas. However, the elderly, dieters, and those on low protein diets often do not consume enough phosphorus to meet the needs of new bone formation.
- SILICON. It has long been known that bioactive silicon (silica) plays an important role in bone collagen synthesis. A 2005 human study found bioactive silicon to enhance the effects of calcium and vitamin D3 on new bone formation.
5. Enhance vitamin intake
While protein and minerals may be the building blocks, vitamins are the catalysts for many biochemical reactions and are equally important. In fracture healing, we can clearly identify the vital roles of several vitamins including vitamin C, vitamin D, and vitamin K as well as the energy-producing B vitamins, which should all be taken in therapeutic doses:
- VITAMIN C is essential for proper synthesis of the bone collagen protein matrix. It is also one of the most important antioxidants and anti-inflammatory nutrients. In severe vitamin C deficiency, collagen becomes too unstable to function properly, which results in skin lesions and fragile blood vessels with eventual bleeding from all mucous membranes. A tendency to black and blue without reason is most often a sign of sub-clinical vitamin C deficiency. Because of its essential role in bone collagen formation, adequate vitamin C is required for fracture healing. Several animal studies document this fact. For example, a small Turkish rat study showed that vitamin C supplementation accelerated the fracture healing process. A similar, yet larger, Spanish study also documented that rats with higher vitamin C blood levels developed a stronger fracture callus than did those with low blood levels.
- VITAMIN D is the primary regulator of calcium absorption and without adequate vitamin D calcium blood level drops making less calcium available for fracture healing. Studies as early as 1945 documented that low vitamin D levels led to suboptimal fracture healing and the administration of vitamin D accelerated initial fracture callus mineralization. Further, we now know that vitamin D, in conjunction with vitamin K, stimulates the transformation of fracture site stem cells to bone building osteoblasts. Overall, vitamin D is central to fracture healing and vitamin D status has been shown to be an independent predicator of functional recovery after hip fracture.
- VITAMIN K is an essential part of the biochemical processes that bind calcium to bone and it is required for proper formation of the osteocalcin bone protein. In addition, vitamin K helps conserve calcium by reducing the loss of calcium in the urine. Since 1960 it has been noted that vitamin K has a beneficial effect on fracture healing and has a real effect on all collagen tissues, especially bone tissue. Researchers have found that vitamin K is sequestered to the site of fracture resulting in markedly depressed circulating levels of vitamin K in fracture patients. The time taken for the vitamin K blood level to return to normal appears to be influenced by the severity of the fracture.
- VITAMIN B6 is one of the B vitamins that has been linked to fracture healing. Animals deficient in this vitamin fracture more frequently and experience reduced fracture healing. It appears that vitamin B6 modulates the effects of vitamin K on bone through complex biochemical pathways.
Anti-inflammatory nutrients help reduce pain
Where there is pain, there is inflammation — a product of the body’s action to tear down, recycle, and repair damaged tissues. For fracture healing, it is ideal to use nutrients that are both anti-inflammatory and nourishing to new bone growth. Useful anti-inflammatory nutrients include vitamin C, quercitin and other flavonoids, omega-3 fatty acids, and proteolytic enzymes such as bromalain and trypsin.
Multi-nutrient therapy is the likely best approach
Bone is complex tissue that requires many nutrients. Given this fact, supplementation with a wide range of key bone nutrients is likely to provide more effective fracture healing than individual nutrient supplementation. At the Center for Better Bones, we always recommend therapeutic doses of all the 20 key bone-building nutrients for optimum fracture healing. While no scientist has yet conducted a clinical trial using all 20 key nutrients for fracture healing, several studies have found multi-nutrient therapy to reduce complication and accelerate fracture healing. A 2006 Swedish hip fracture study found fracture patients given complex multi-nutrient supplementation containing protein, carbohydrates, amino acids, sodium, potassium, calcium, magnesium, chloride, trace minerals, and fat soluble vitamins, had only a 15% rate of complications as compared to a 70% complications rate among the non-supplemented group. Also impressive is a Swedish meta-analysis of 17 such clinical hip fracture trials which reported that oral multi-nutrient supplementation (including nutrients such as carbohydrates, protein, arginine, zinc, and antioxidants) reduced deaths and complications from hip fracture by nearly 50%.
Another innovative placebo controlled, multi-nutrient study from India administered vitamin C, lysine, proline, and vitamin B6 to tibial fracture patients. In those receiving multi-nutrient therapy, fracture healing time was reduced by approximately two weeks, with a larger percentage healing in 10 weeks (33%) as compared to the 11% in the placebo group.
An Alkaline for Life® eating program stimulates bone repair
The Alkaline for Life® eating program provides a diet rich in minerals, vitamins, and phytonutrients obtained from vegetables, fruits, nuts, and seeds. This life-supporting eating pattern has been shown to create a health-promoting internal biochemical environment which, among other things, conserves bone building minerals and proteins. Such a base-forming eating program also has been shown to increase growth hormones and growth factors such as IGF insulin-like growth factor. These growth hormones are among the most important biochemical forces encouraging fracture repair and new bone formation.
Herbal fracture healing aids
Throughout history, and even today in much of the world, traditional herbal medicine has been the mainstay of medical practice. This long tradition of herbal wisdom has employed various herbs to speed fracture healing. Among these is cultivated (European) comfrey (Symphytum uplandics x.), which should not be confused with a potentially toxic wild variety (Symphytum officinale), nor with a native herb that is also called “wild comfrey” (Cynoglossum virginianum) that is native to the US. Herbalist Susun Weed recommends cultivated comfrey be used as an aid in fracture healing. Details of her recommendation are available at www.susunweed.com/herbal_ezine/June08/wisewoman.htm). She also reports great success applying a hot, fresh burdock leaf poultice to reduce the swelling induced by a fracture. Arnica (Arnica montana) is reportedly another helpful herb, as detailed by herbal researcher Alma Hutchens, but it must be used with caution as large amounts are poisonous. She reports that five drops or fewer of Arnica tincture given every 3 to 4 hours after the initial trauma is said to help recovery from the trauma of fracture. Horsetailgrass is an herb high in silicon, which can be boiled and made into a tea valuable in the early stages of fracture healing. In all cases, however, herbal medicine should be used under the guidance of a qualified herbalist.
Traditional Chinese herbal medicine can be an effective way to reduce the swelling, pain, and soreness of fracture. Chinese medicine can also accelerate healing when used under the guidance of an experienced practitioner. Finally, the traditional Ayurvedic medicine of India is now becoming known in the West and drawing the attention of scientists and pharmaceutical companies alike. The Indian herb Cissus quadrangularisin particular has been studied for its fracture-healing benefits.
As we look around the world, we would indeed expect to find traditional herbal approaches to fracture healing and those with access to an expert herbalist can benefit from this traditional wisdom.
Exercise and fracture healing
Exercise is unlikely to pop into your mind as an important way to accelerate fracture healing — yet it is. In general, bone tissue responds to patterns of loading by increasing matrix synthesis, altering composition, organization, and mechanical properties. Evidence indicates that the same holds true for bone under repair. Further, fracture healing requires good circulation and an adequate flow of nutrient-replenishing blood to the fracture site — both of which are enhanced by exercise. To avoid stress on the broken bone, joint loading, range of motion, and specific tendon-gliding exercises are employed to accelerate healing and assure return of function post fracture. For example, in the case of a broken forearm, exercises would involve movements of the fingers and hand, as well as the elbow and shoulder joints.
Energy medicine for fracture healing
Energy medicine is described in a recent medical journal as, “…a field of complementary therapy based on the interactions of the human energy field with other energy fields (human or other).” Interestingly enough, pulsing electromagnetic field therapy is a form of energy medicine that has been used for many years by conventional doctors to heal fractures that have not healed on their own (known as non-union fractures). Approximately 5 — 10% of bone fractures fail to heal normally and result in delayed healing or non-union. In these situations, the use of electromagnetic bone stimulating devices has proven to speed healing. For a review of the literature see: www.ifess.org/Services/Consumer_Ed/References/bone_healing_references.htm
Homeopathy, reiki, qi gong, polarity therapy, healing touch, acupuncture, and massage are all non-conventional energy healing modalities with applications for fracture healing. Common over-the-counter homeopathic remedies include arnica as an anti-trauma remedy for immediately after the fracture (not to be used if the person is unconscious), symphytum (comfrey) for pain relief and the joining of set bones, and Calcarea phosphorica for fractures that are difficult to heal. Low-potency homeopathic remedies (6x, 6c to 30x, 30c) are often used for self-help, as detailed in Homeopathic Self-Care by Robert Ullman and Judyth Reichenberg-Ullman (Prima Publishing, 1997) and at www.peacehealth.org/kbase/cam/hn-2201007. Homeopathy is a powerful medicine and when possible the best policy is to seek the advice of a professional homeopath.
Pain relievers and fracture healing
Cells damaged from the trauma of fracture release large amounts of inflammatory prostaglandins at the site of fracture. The ensuing inflammation causes pain and the natural tendency is to want to block this painful reaction. In this case, non-steroidal anti-inflammatory drugs (COX-1 and COX-2 inhibitors) might be the medication we reach for to relieve the pain. The use of these COX-1 and COX-2 inhibitors, however, can delay fracture healing. As it turns out, prostaglandin-induced inflammation is an essential component of the fracture healing process, and cyclooxygenase enzymes (COX-1 and COX-2) play important roles in fracture repair. These inflammatory prostaglandins are a natural and essential part of initial tissue repair and the initial inflammatory immune response is crucial to fracture healing. Because of this, the use of non-steroidal anti-inflammatory pain killers (NSAIDs) is not recommended for fracture pain relief. Among the NSAID COX-1 and COX-2 inhibitor drugs to be avoided are aspirin, ibuprofen, indomethacin, etodolac (Lodine), meloxicam (Mobic), nabumetone (Relafen), and naproxen (Anaprox, Naprosyn).
Acceptable alternatives to help reduce the pain of fracture include acetaminophen (as in Tylenol). In severe cases, narcotics such as codeine are given along with the acetaminophen. There are also natural pain-relief alternatives, including several nutrients that have been documented to help reduce the pain of inflammation of fracture while also enhancing the healing process. For example, in a study of 328 wrist fracture patients, modest 500 mg/day supplementation with vitamin C reduced by more than 4-fold the incidence of post-fracture complex regional pain syndrome. In clinical use at the Center for Better Bones, we have found that the well-studied flavonoid, quercitin, used in doses of 2–3 g per day, has a synergistic effect with vitamin C, amplifying the pain-relief benefits. These nutrients, as well as omega-3 fatty acids, reduce inflammation without inhibiting the COX-1 and COX-2 enzymes. In addition, European research has shown the value of proteolitic enzymes (protein digesting enzymes) such as bromelain and trypsin for reducing inflammation, edema, and pain in fracture patients. One such European proteolytic enzyme combination available in the US is the Wobenzym formula.
Smoking
Numerous studies document that smoking delays the healing process and increases morbidity associated with fracture. For example, the fractured tibias of patients who smoked took 62% longer to heal than non-smokers. Further, postoperative complications such as delayed healing, infection, and fracture non-healing (non-union) are much more common among smokers.
A further example from a study at Johns Hopkins University found that:
- Current and previous smokers were less likely to achieve union than non-smokers.
- Current smokers were more than twice as likely to develop an infection.
- Previous smokers were 2.8 times more likely to develop osteomyelitis (bone infection).
Interestingly enough, the impact of smoking appears to be a non-nicotine effect involving delays in the cartilage-forming phase of fracture healing. All in all, the clear recommendation is that those who fracture cease smoking for the full rehabilitation period.
Alcohol abuse
Alcohol in excess can be directly toxic to bone and alcohol abuse is associated with increases in both the incidence of fractures and complications of fracture healing, including infection. In a Danish ankle fracture study, for example, alcohol abusers had significantly more early complications, especially infections, from reparative ankle surgery. It is highly advisable to eliminate any excessive alcohol intake during fracture healing.
Conclusion
Bone is a complex, living tissue which constantly changes and adapts itself to the demands put upon it. A myriad of nutrients, hormones, and other biochemical factors are essential to bone formation and maintenance, so an equal number of factors figure in the bone repair process. While a fracture can be frightening and leave us questioning the strength of our skeleton, such a mishap might well be seen as a “window of opportunity” to make nutritional and lifestyle changes that will strengthen the entire skeleton and improve overall health.
I came to Dr. Brown through the internet, many months after having been hit by a car on my bike. My leg had been badly broken in several places, and a year later I still had a complete “nonunion” of the tibia and fibula. Betterbones.com was the only nutritionally based service for supporting bone rebuilding that I could find and so I began consultations with Dr. Brown. With a solid footing in research evidence, she assessed my particular situation and guided me in adding specific bone-building supplements as well as making dietary adjustments and including complementary treatments. I recently had a surgical follow-up to my sixth round of orthopedic surgery, and at six months the bones are substantially healed. My surgeon was thrilled ( and surprised!), and of course I am ecstatic. ( I came pretty close to having my leg amputated) I have no doubt that Dr. brown’s work in the background helped with my phenomenal healing success. I should mention that I am 50 years old, and that long term unhealed bone injuries as well as ones that are distal (lower extremities) are notoriously hard to heal. Thank You, Dr. Brown!
