All About the C5-C6 Spinal Motion Segment
If the pain comes from the degenerative disc itself, then it will likely go away on its own within a few weeks or months. However, other symptoms of cervical degenerative disc disease are more likely to become chronic and require treatment if facet joints in the neck also start to degenerate and/or a spinal nerve becomes pinched.
Cervical Degenerative Disc Disease Symptoms and Diagnosis
Symptoms of cervical degenerative disc disease can vary widely from person to person.
When cervical degenerative disc disease becomes symptomatic, the pain might develop slowly over time or appear suddenly. The symptoms can range from mildly annoying neck discomfort to debilitating pain, numbness, and/or weakness that radiates into the arm and hand.
Common Cervical Degenerative Disc Disease Symptoms
Some common characteristics of cervical DDD symptoms include:
- Neck pain. The low-grade pain of a stiff neck is the most common symptom of cervical degenerative disc disease. However, sometimes the pain could also flare up and become severe, perhaps lasting a few hours or days. See Stiff Neck Causes, Symptoms, and Treatment
- Nerve pain. This type of pain tends to be sharp or electric shock-like and can radiate down the shoulder into the arm, hand, and/or fingers. Typically, nerve pain would only be felt on one side of the body. See Could That Shoulder Pain Really Stem From the Neck?
- Neurological symptoms in the arm, hand, and/or fingers. Pins-and-needles tingling, numbness, and/or weakness can radiate down the shoulder into the arm, hand, and/or fingers. These types of symptoms can interfere with daily activities, such as typing, getting dressed, or holding objects. See Understanding Hand Pain and Numbness
- Pain gets worse with movement. In general, pain caused by the degenerative disc itself tends to be aggravated by movement and alleviated by rest.
If the pain comes from the degenerative disc itself, then it will likely go away on its own within a few weeks or months. However, other symptoms of cervical degenerative disc disease are more likely to become chronic and require treatment if facet joints in the neck also start to degenerate and/or a spinal nerve becomes pinched.
In This Article:
- Cervical Degenerative Disc Disease
- Cervical Degenerative Disc Disease Symptoms and Diagnosis
- How Cervical Degenerative Disc Disease Causes Pain and Other Symptoms
- Cervical Degenerative Disc Disease Treatment Options
- Cervical Degenerative Disc Disease Video
Less Common Cervical Degenerative Disc Disease Symptoms
The more the cervical spine degenerates, the more likely the spinal canal will narrow and put the spinal cord at risk. If the spinal cord becomes compressed, then myelopathy could result and include symptoms such as:
- Difficulty moving arms and/or legs
- Trouble with coordination and/or balance
- Loss of bowel and/or bladder control
- Weakness and/or numbness anywhere beneath the neck
- Shock-like pains through the arms or legs, which can be made worse by bending forward
Cervical myelopathy is cause for concern and requires prompt medical attention. It usually occurs in people over age 50.
Diagnosing Cervical Degenerative Disc Disease
The condition is typically diagnosed by the following process:
- Medical history. First, a doctor will review the patient’s medical history in addition to learning about the current symptoms.
- Physical examination. Next, a doctor will perform a physical examination by palpating (feeling) the neck and testing the neck’s range of motion. During the exam, patients may be asked to perform certain movements and report whether the neck pain increases or decreases. If the pain is severe or if neurological symptoms are present, such as pain, tingling, or weakness in the shoulder, arm, or hand, then the doctor will likely request an imaging study.
- Imaging confirmation. If the doctor determines that an imaging study is needed to check for a potential disc problem, then an MRI will likely be ordered. An MRI, X-ray, or possibly a CT scan can confirm whether and where degeneration is occurring, as well as identify other conditions (such as osteoarthritis or stenosis) that might be causing the symptoms.
Once an accurate diagnosis of cervical degenerative disc disease is confirmed, as well as any other associated conditions, then the source of the symptoms can be understood and an effective treatment program can be created.
All About the C5-C6 Spinal Motion Segment
The C5-C6 spinal motion segment (located in the lower cervical spine just above the C7 vertebra) provides flexibility and support to much of the neck and the head above. Due to its high load-bearing function, the C5-C6 motion segment is frequently affected by poor posture, degeneration, disc herniation, radicular pain, and trauma. 1 Gray JC, Grimsby O. Interrelationship of the spine, rib cage, and shoulder. In: Donatelli RA. Physical Therapy of the Shoulder. 5th ed. London: Churchill Livingstone; 2012: 87-130. , 2 Quraishi NA, Elsayed S. A traumatic, high-energy and unstable fracture of the C5 vertebra managed with kyphoplasty: a previously unreported case. Eur Spine J. 2011;20(10):1589-92. , 3 Binder AI. Cervical spondylosis and neck pain. BMJ. 2007;334(7592):527-31. , 4 Haghnegahdar A, Sedighi M. An Outcome Study of Anterior Cervical Discectomy and Fusion among Iranian Population. Neurosci J. 2016;2016:4654109. , 5 Boyles R, Toy P, Mellon J, Hayes M, Hammer B. Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. J Man Manip Ther. 2011;19(3):135-42.
Anatomy of the C5-C6 Spinal Motion Segment
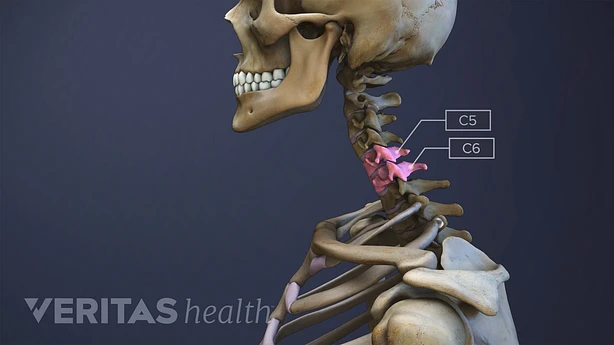
The C5-C6 spinal motion segment includes the C5 and C6 vertebrae, the intervertebral disc, and the adjacent connective tissues. The C6 spinal nerve exits the spinal cord through the intervertebral foramen above the C6 vertebra. Watch: Spinal Motion Segment: C5-C6 Video
The C5-C6 spinal motion segment includes the following structures:
- C5 and C6 vertebrae. These vertebrae are each composed of a vertebral body, a vertebral arch, and 2 transverse processes. Together they form paired, synovial facet joints with gliding movements. Articulating cartilages are present on the joint surfaces to provide smooth movements and prevent friction between the facet joint surfaces of C5 and C6 vertebrae at the back. The vertebrae are held together with ligaments that attach one vertebra to the other at various attachment points. See Cervical Vertebrae
- C5-C6 intervertebral disc. A disc made of a gel-like material (nucleus pulposus) surrounded by a thick fibrous ring (annulus fibrosus) is situated between the vertebral bodies of C5 and C6. This disc provides cushioning and shock-absorbing functions to protect the vertebrae from grinding against each other during neck movements, while also allowing movement in all directions. See Cervical Discs
- C6 spinal nerve. In between C5-C6, the C6 spinal nerve exits the spinal cord through a small bony opening on the left and right sides of the spinal canal called the intervertebral foramen. This C6 nerve has a sensory root and a motor root.
- The C6 dermatome is an area of skin that receives sensations through the C6 nerve. This dermatome includes the skin over the ‘thumb’ side of the forearm and the thumb.
- The C6 myotome is a group of muscles controlled by the C6 nerve. These muscles include the wrist extensor muscles, which allow the wrist to bend backward; and the biceps and supinator muscles of the upper arm, which serve to bend the elbow and rotate the forearm.
The spinal cord is protected within the spinal canal, with the vertebral bodies in front and vertebral arches at the back. The vertebral arteries are protected by bony tunnels going up either side of the vertebrae.
Common Problems at C5-C6
The C5-C6 motion segment is prone to the following injuries and disorders:
- Disc problems. Herniation of the C5-C6 intervertebral disc is common. 4 Haghnegahdar A, Sedighi M. An Outcome Study of Anterior Cervical Discectomy and Fusion among Iranian Population. Neurosci J. 2016;2016:4654109. This condition may result due to the shearing forces that affect the disc when the head drifts forward from poor posture. 1 Gray JC, Grimsby O. Interrelationship of the spine, rib cage, and shoulder. In: Donatelli RA. Physical Therapy of the Shoulder. 5th ed. London: Churchill Livingstone; 2012: 87-130. Herniation may also result from injury or aging-related wear and tear. The C5-C6 disc may also be subject to traumatic degeneration following a whiplash injury in some cases. 6 Kongsted A, Sorensen JS, Andersen H, Keseler B, Jensen TS, Bendix T. Are early MRI findings correlated with long-lasting symptoms following whiplash injury? A prospective trial with 1-year follow-up. Eur Spine J. 2008;17(8):996-1005. Problems to this disc are often a source of C6 radicular nerve pain. 3 Binder AI. Cervical spondylosis and neck pain. BMJ. 2007;334(7592):527-31. , 5 Boyles R, Toy P, Mellon J, Hayes M, Hammer B. Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. J Man Manip Ther. 2011;19(3):135-42. See All About Spinal Disc Problems
- Spondylosis. Spondylosis (degeneration) of the C5-C6 vertebrae and intervertebral disc occurs at a higher rate compared to other cervical vertebrae. 3 Binder AI. Cervical spondylosis and neck pain. BMJ. 2007;334(7592):527-31. Spondylosis usually results in the formation of bone spurs (osteophytes), eventually leading to stenosis or narrowing of the intervertebral foramina or spinal canal. Watch Cervical Spondylosis with Myelopathy Animation
- Fracture. Research suggests about 20% of traumatic neck fractures occur at the C6 vertebral level and 15% occur at C5. 2 Quraishi NA, Elsayed S. A traumatic, high-energy and unstable fracture of the C5 vertebra managed with kyphoplasty: a previously unreported case. Eur Spine J. 2011;20(10):1589-92. Motor vehicle accidents or trauma causing forceful bending of the neck forward or backward, such as in whiplash, may cause these fractures, leading to instability of the neck and injury to the nerve roots or the spinal cord.
- Congenital stenosis. The C5 vertebra is at a greater risk for spinal canal stenosis as an inherited genetic trait compared to other vertebrae lower in the cervical spine. 7 Nehete LS, Bhat DI, Gopalakrishnan MS, et al. Unusual cause of high cervical myelopathy-C1 arch stenosis. J Craniovertebr Junction Spine. 2018;9(1):37-43.
Rarely, tumors and infections may affect the C5-C6 vertebrae and spinal segment.
In This Article:
- All About the C5-C6 Spinal Motion Segment
- C5-C6 Treatment
- Spinal Motion Segment: C5-C6 Video
Common Symptoms and Signs Stemming from C5-C6
Vertebral and disc pain from C5-C6 may occur suddenly following an injury or gradually increase over a period of time. Typically, a dull ache or sharp pain may be felt at the back of the neck. The neck’s range of motion may also decrease. There may be crepitus (a snap, crackle, or pop sound) with neck movements.
Compression or inflammation of the C6 spinal nerve is common 3 Binder AI. Cervical spondylosis and neck pain. BMJ. 2007;334(7592):527-31. , 5 Boyles R, Toy P, Mellon J, Hayes M, Hammer B. Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. J Man Manip Ther. 2011;19(3):135-42. and may cause additional symptoms such as:
- Pain in the shoulder, upper arm, forearm, hand, thumb, and index finger; frequently aggravated by arm or neck movements. 8 Ngnitewe Massa R, Mesfin FB. Herniation, Disc. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/ , 9 Radpasand M. Use of a multimodal conservative management protocol for the treatment of a patient with cervical radiculopathy. J Chiropr Med. 2011;10(1):36-46. Sometimes, the pain may also radiate from the neck into the arm. 9 Radpasand M. Use of a multimodal conservative management protocol for the treatment of a patient with cervical radiculopathy. J Chiropr Med. 2011;10(1):36-46.
- Numbness in the outer side of the forearm, thumb, and index finger. 8 Ngnitewe Massa R, Mesfin FB. Herniation, Disc. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/
- Weakness in the shoulder, elbow, and wrist, commonly affecting the motion of these joints. 8 Ngnitewe Massa R, Mesfin FB. Herniation, Disc. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/ , 10 Seo TG, Kim du H, Kim IS, Son ES. Does C5 or C6 Radiculopathy Affect the Signal Intensity of the Brachial Plexus on Magnetic Resonance Neurography?. Ann Rehabil Med. 2016;40(2):362-7.
Symptoms may occur on one or both sides of the body.
An injury to the spinal cord at the C5-C6 level may cause pain, weakness, or paralysis in the arms and/or legs. There may be loss of bowel and bladder control or breathing problems in some cases.
Nonsurgical treatments are often tried first for pain that stems from C5-C6. In rare cases, surgery may be considered.
- 1 Gray JC, Grimsby O. Interrelationship of the spine, rib cage, and shoulder. In: Donatelli RA. Physical Therapy of the Shoulder. 5th ed. London: Churchill Livingstone; 2012: 87-130.
- 2 Quraishi NA, Elsayed S. A traumatic, high-energy and unstable fracture of the C5 vertebra managed with kyphoplasty: a previously unreported case. Eur Spine J. 2011;20(10):1589-92.
- 3 Binder AI. Cervical spondylosis and neck pain. BMJ. 2007;334(7592):527-31.
- 4 Haghnegahdar A, Sedighi M. An Outcome Study of Anterior Cervical Discectomy and Fusion among Iranian Population. Neurosci J. 2016;2016:4654109.
- 5 Boyles R, Toy P, Mellon J, Hayes M, Hammer B. Effectiveness of manual physical therapy in the treatment of cervical radiculopathy: a systematic review. J Man Manip Ther. 2011;19(3):135-42.
- 6 Kongsted A, Sorensen JS, Andersen H, Keseler B, Jensen TS, Bendix T. Are early MRI findings correlated with long-lasting symptoms following whiplash injury? A prospective trial with 1-year follow-up. Eur Spine J. 2008;17(8):996-1005.
- 7 Nehete LS, Bhat DI, Gopalakrishnan MS, et al. Unusual cause of high cervical myelopathy-C1 arch stenosis. J Craniovertebr Junction Spine. 2018;9(1):37-43.
- 8 Ngnitewe Massa R, Mesfin FB. Herniation, Disc. [Updated 2018 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441822/
- 9 Radpasand M. Use of a multimodal conservative management protocol for the treatment of a patient with cervical radiculopathy. J Chiropr Med. 2011;10(1):36-46.
- 10 Seo TG, Kim du H, Kim IS, Son ES. Does C5 or C6 Radiculopathy Affect the Signal Intensity of the Brachial Plexus on Magnetic Resonance Neurography?. Ann Rehabil Med. 2016;40(2):362-7.






