Coughing Up Phlegm
The Ohio State University Wexner Medical Center: “What Does the Color of Phlegm Mean?”
Brown Phlegm: What Causes It?
Phlegm. Mucus. Sputum. These are different names for the slimy, slippery stuff that flows out when you cough, sneeze, or sniffle.
This gunk is your body’s defense weapon against infectious microbes and allergens that irritate your lungs or sinuses. The color and texture can vary widely, from clear sticky strings to stretchy yellow messes to thick green clots.
Brown phlegm is less common. Here are some reasons why you might get it.
It can be a sign of old blood, chronic — ongoing — inflammation, or tar that loosens up after you’ve quit smoking.
COPD
Chronic obstructive pulmonary disease happens when your lungs get so swollen over time that air can’t flow freely. Cigarette smoke is usually the reason. You might cough, wheeze, and have trouble breathing. If your mucus turns brown, yellow, or green, it can be an early warning sign of a flare-up. It’ll be stickier and thicker, and there’ll be more of it.
Treatments for COPD include medications, pulmonary rehab, supplemental oxygen, and surgery to open up blocked pathways. In severe cases, you may need a lung transplant.
Acute Bronchitis
This is when the linings of your bronchial tubes, the air passageways in your lungs, get inflamed. Viral infections are the most common cause of acute bronchitis. But it also can be brought on by bacteria, an irritant such as smoking, an allergy, or certain chemicals.
If you have it, you’ll first notice a cough. It could be dry or bring up phlegm. The mucus can range from clear to cloudy, brown, yellow, or green. Your chest might feel tight or tender. Other signs are a fever, tiredness, shortness of breath, a sore throat, and a stuffy nose.
Bronchitis usually goes away on its own. Your doctor might suggest ways to thin out your mucus to make it easy to cough up. You can run a vaporizer, stand in a hot shower, or hover over a steam tent over hot water. If your symptoms don’t go away and your doctor strongly suspects a bacterial infection, they may prescribe an antibiotic.
Bacterial Pneumonia
A dry cough that brings up thick phlegm is one of the main symptoms of pneumonia. The mucus might be yellow, green, red, brown, or rust-colored. Sometimes the color can be a tip-off of the type of bacteria that caused the illness.
Pneumonia starts with tissue swelling in one or both of your lungs. The tiny grape cluster-like air sacs at the tips of your breathing tubes can swell and fill up with fluid. You’ll need antibiotics to treat bacterial pneumonia.
Chronic Lung Disease
This term includes a wide range of lung disorders that don’t go away or worsen over time. They can be hereditary, be triggered by things in the environment, or start with a habit like smoking.
Two forms of chronic lung disease, cystic fibrosis (CF) and bronchiectasis, might lead you to cough up clingy, dark-brown phlegm.
Cystic fibrosis. People with CF are born with a faulty gene that makes their mucus very thick and sticky. Instead of lubricating, the phlegm clogs the lungs and holds onto germs that lead to lingering infections. Adults with CF often may cough up mucus that’s tinged with blood. That can happen if repeated infections irritate a small blood vessel.
CF is a lifelong condition. Treatment includes techniques to keep the airways clear and break up mucus, inhalers, antibiotics, enzyme supplements, and targeted fitness programs that boost energy and help your lungs work better.
Bronchiectasis. This happens if the airways that join your windpipe to the lower part of your lungs are too wide. Mucus can build up and make you more likely get lung infections. Bronchiectasis can result from such conditions as childhood whooping cough, pneumonia, severe asthma, and COPD. A main symptom is mucus in a variety of shades, from white to brown.
Since bronchiectasis is a long-term condition, you may need to stay on inhalers and other drugs to lower your swelling. Antibiotics and flu vaccines can help prevent infections.
Fungus Allergy
Aspergillus is a fungus that’s widely found in soil, plants, and rotting vegetation. If you’re allergic and breathe it in, it can inflame your lungs. You might wheeze and cough up brown-flecked mucus. You might get a fever. If you have cystic fibrosis or asthma, you’re more likely to have this allergy. If so, your doctor will call it allergic bronchopulmonary aspergillosis.
Your doctor may prescribe medications that help tame inflammation, as well as antifungal drugs.
Lung Abscess
This is a painful pocket of pus wrapped in inflamed tissue. It can happen if the bacteria in your mouth or throat, such as from gum disease, gets down to your lungs. If you can’t cough it out, infection can set in and form a cavity.
Your symptoms will start slowly. You might feel tired, have night sweats or fever, and cough up foul-smelling, brown- or blood-specked phlegm. You’ll need a course of antibiotics over at least a few weeks to clear it up.
Quitting Smoking
Within a week after your last cigarette, your lungs start cleaning themselves. Smoke slows down the tiny cilia that sweep mucus from your lungs. Once they can do their job right, you might start to cough up brown mucus from the tar you’ve inhaled over time. This might go on for a few weeks. You can help get rid of it faster by drinking lots of fluids and running a humidifier or vaporizer to help moisten and thin out your phlegm.
If your cough lasts more than a month or if you see blood, see your doctor.
Show Sources
Harvard University: “All About That Mucus: How It Keeps Us Healthy.”
The Ohio State University Wexner Medical Center: “What Does the Color of Phlegm Mean?”
Western Australia Department of Health: “Facts About Giving Up Smoking.”
Mayo Clinic: “COPD.”
Breathe: The Lung Association (Canada): “Recognize the Early Warning Signs of a Flare-up.”
American Lung Association: “Treating COPD,” “The Basics of Pulmonary Rehabilitation.”
Harvard Medical School: “Acute Bronchitis.”
Medscape: “Bacterial Pneumonia.”
National Health Service (UK): “Pneumonia.”
John Muir Health: “Chronic Lung Disease.”
Cystic Fibrosis Foundation: “About Cystic Fibrosis.”
Mount Nittany Health: “Allergic Bronchopulmonary Aspergillosis.”
Merck Manuals: “Abscess in the Lungs.”
BMJ Case Reports: “Unusual case of a lung abscess.”
Mayo Clinic: “Quit Smoking FAQ.”
Coughing Up Phlegm
Coughing up phlegm is a normal symptom of colds and other health conditions. But coughing up phlegm without feeling sick could indicate a more serious underlying issue like heart or lung disease.
- Northeast Ohio 216.444.8500
- Appointments & Locations
- Request an Appointment
Overview
What is coughing up phlegm?
Coughing up phlegm is a symptom of infections like the flu and common cold. Phlegm is a specific type of mucus that originates in your lungs and throat. It’s slightly thicker than the mucus that’s produced in your nose and sinuses. Another name for phlegm is sputum.
Most of the time, coughing up phlegm isn’t a cause for concern. It helps clear irritants and infections from your lungs. But if you cough up phlegm when you’re not feeling sick, it could mean you have a more serious underlying health condition. It can also tell you a lot about what’s going on with your body.
Possible Causes
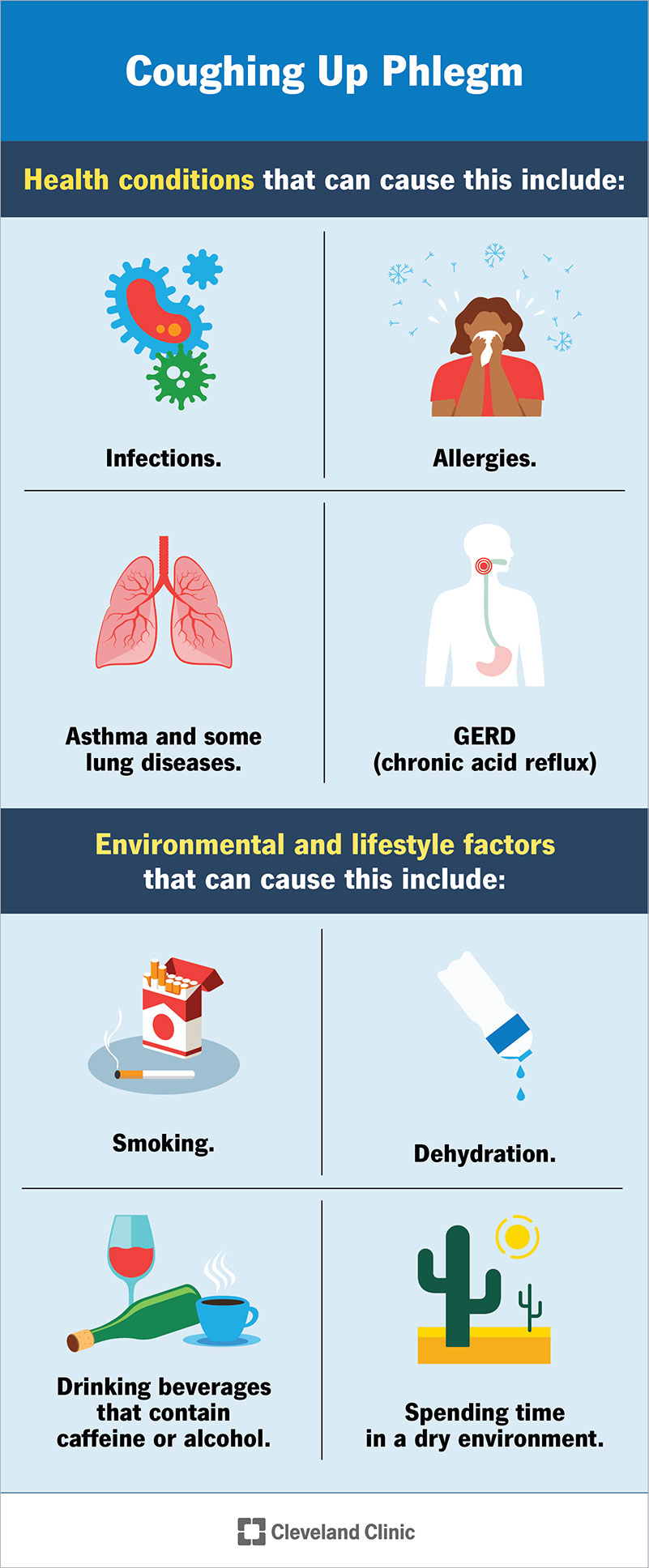
What causes coughing up phlegm?
There are several health conditions — ranging from mild to severe — that can result in coughing up phlegm, including:
- Infections.
- Allergies.
- Asthma.
- GERD (chronic acid reflux).
- Lung diseases, such as COPD.
Certain environmental and lifestyle factors can contribute to coughing up phlegm, too, including:
- Smoking.
- Drinking beverages that contain caffeine or alcohol.
- Dehydration.
- Spending time in a dry environment.
What does it mean when you cough phlegm up?
Coughing up phlegm could mean different things depending on the color and consistency of the mucus. But you should always check with a healthcare provider if something doesn’t seem right.
Coughing up clear phlegm
If you’re coughing up clear phlegm, it usually means your body is trying to flush out pollen, pet dander or other allergens. However, in some cases, it could indicate a more serious condition, such as:
- Viral bronchitis.
- Viral pneumonia.
Coughing up yellow or green phlegm
This usually means your body is fighting off some sort of infection. People often develop yellow phlegm in the early stages, and it turns green the longer the infection lingers. Possible health conditions related to coughing up yellow or green phlegm include:
Coughing up white phlegm
White phlegm can mean a few different things, including:
- GERD.
- COPD.
- Viral bronchitis.
- Congestive heart failure. (If you develop heart failure symptoms, like shortness of breath, fatigue or leg weakness, call a healthcare provider immediately.)
Coughing up black phlegm
Another name for black phlegm is melanoptysis. Common causes include:
- Smoking.
- Breathing in coal dust or other dark materials or toxins.
- Exophiala dermatitidis, a type of fungal infection.
Coughing up brown phlegm or phlegm with brown spots
When you see brown phlegm, rust-colored phlegm or phlegm with brown spots, it usually indicates old blood. Common related conditions include:
- Bacterial bronchitis.
- Bacterial pneumonia.
- Cystic fibrosis.
- Lung abscess.
- Breathing in dust or other brown materials or toxins.
Coughing up bloody phlegm, red phlegm or pink phlegm
Coughing up bloody phlegm indicates a more serious issue. Common causes of red phlegm include:
- Pneumonia.
- Pulmonary embolism.
- Congestive heart failure. (Symptoms include pink, frothy phlegm, chest pain, sweating and shortness of breath.)
- Tuberculosis.
- Lung cancer.
If you cough up blood without phlegm, call a healthcare provider immediately or head to your nearest emergency room.
Care and Treatment
How do you stop coughing up phlegm?
Treatment depends on the underlying cause. For instance, if you’re coughing up phlegm as a result of allergies, your healthcare provider may recommend decongestants, antihistamines or corticosteroids. If you have an infection, your provider may prescribe antibiotics. If GERD causes you to cough up phlegm, then you might need antacids or other medications that relieve acid reflux symptoms.
Your cough may go away on its own in a few days. But if you’ve been coughing up phlegm for two weeks or more and your symptoms haven’t improved, schedule an appointment with a healthcare provider.
Are there things I can do at home to encourage coughing up phlegm?
Coughing up phlegm helps rid your body of allergens, irritants and infections. Here are some recommendations on how to cough up phlegm:
- Use ahumidifier. Keeping the air in your home moist can help loosen phlegm in your lungs so you can cough it up easier.
- Stay hydrated.Drink plenty of water to help thin out mucus and prevent dehydration.
- Gargle with saltwater. Add 1/2 tablespoon of salt to a glass of warm water. Gargle to loosen any phlegm.
- Take over-the-counterexpectorants. Expectorants (like Mucinex®) thin your mucus so it’s easier to cough up.
- Use eucalyptus oil. Products containing eucalyptus oil (like Vicks® VapoRub™) can help loosen phlegm in your chest. Use these products exactly as described on the label.
When to Call the Doctor
When should I see my healthcare provider?
You should schedule an appointment with a healthcare provider if:
- Your cough lasts for more than two weeks.
- You’re coughing up phlegm that’s not clear in color.
- You have a fever.
- You’re wheezing or having difficulty breathing.
Frequently Asked Questions
Is coughing up phlegm a good thing?
Yes. While the presence of mucus may indicate an underlying issue, coughing up phlegm is a good thing because it helps clear irritants, allergens and infections out of your system.
Is coughing up phlegm a symptom of COVID-19?
Currently, research suggests that most people who get COVID-19 develop a dry cough. However, as the virus worsens, some people may notice an increase in mucus production and may cough up phlegm as a result.
When should I be worried about coughing up phlegm?
Coughing up phlegm is a good thing. But if your cough lasts longer than two weeks or if the phlegm is yellow, green, brown, black, white or red, you should schedule an appointment with a healthcare provider as soon as possible.
If you’re coughing up blood without phlegm, call a healthcare provider right away or go to your nearest emergency room.
A note from Cleveland Clinic
Coughing up phlegm is unpleasant. Examining it, even more so. But phlegm can tell you a lot about what’s going on inside your body. If you cough up phlegm that’s yellow, green, brown, black, white or red — or if you cough up mucus for two weeks or longer, schedule a visit with your healthcare provider. They can find out what’s causing you to cough up phlegm and treat any underlying conditions.
Brown Mucus/Phlegm Symptoms
Shamard Charles, MD, is a physician-journalist and public health doctor who advances health policy through health communication and health promotion.
Published on October 31, 2022
Susan Russell, MD is a board-certified pulmonologist and currently the Medical Director for Northwestern Memorial Hospital’s Inpatient Pulmonary Unit.
Table of Contents
Table of Contents
Mucus comes in a variety of colors (green, white, reddish-pink, or brown), textures, and even names (such as sputum and phlegm ). Clear or watery phlegm is usually not worrisome. It is associated with benign conditions like seasonal allergies, post-nasal drip, or a cold.
Less commonly, you may find yourself coughing up brown mucus, which may be associated with a number of conditions, including smoking, chronic lung disease, or infections.
The presence of tar, dirt, or old blood or the inflammation of the lower portions of the throat and upper airways are the most common reasons for brown phlegm. This article will explain the symptoms associated with brown mucus, its many causes, and how to treat it.
:max_bytes(150000):strip_icc()/GettyImages-1224255342-747e7afd4051402b937f13b5278cd2fc.jpg)
Symptoms of Brown Mucus/Phlegm
The presence of brown mucus may be worrisome, especially if you are a current or former smoker. The most common symptom associated with brown mucus or phlegm is a cough. A cough associated with any type of mucus is called a productive cough. Other symptoms associated with brown phlegm include:
- Fever
- Chills
- Shortness of breath
- Congestion
- Sneezing or sniffles
- Wheezing
- Chest pain, especially pain on inspiration (breathing in) or expiration (breathing out)
- Sore throat
- Sweating
- Exercise intolerance
- Fatigue
- Unexplained weight loss
Causes of Brown Mucus/Phlegm
If you notice you have brown phlegm, you don’t need to be excessively alarmed, especially if you are young, generally healthy, and have no smoking history or other risk factors.
Still, you should never take the presence of brown phlegm lightly. Get checked by a healthcare provider to make sure that more serious underlying conditions are not the cause of your symptoms.
Brown phlegm can be caused by a wide range of conditions, including:
- Smoker’s cough: Tar from the lungs due to chronic smoking may be brought up with coughing.
- Exposure to air pollution.
- Inhalation of toxic environmental or occupational substances such as coal dust from mining (coal workers’ pneumoconiosis).
- Viral infection.
- Chronic lung disease: Chronic lung diseases like chronic obstructive pulmonary disease, chronic bronchitis, bronchiectasis, and emphysema are often associated with long-term smoking, although genetic conditions like cystic fibrosis and interstitial lung disease may also cause brown mucus.
- Lung cancer: Smoking is the major risk factor for lung cancer, but it can occur in non-smokers. Your risk of lung cancer remains high even 15 years after quitting smoking. Quitting early, before the age of 40, has also been associated with a lower lung cancer risk.
- Bacterial pneumonia: Bacterial infections damage the tissues that line the lungs. Bleeding, especially old blood that remains in the lungs, can taint the mucus in your upper airways and make it appear brown.
- Lung abscess: This is a pocket of infection in the lung, often caused by aspirating material into the lungs. Sometimes a productive cough is the first sign of a lung abscess.
- Asthma (rarely).
How to Treat Brown Mucus/Phlegm
The presence of brown phlegm can be alarming, but if you are generally healthy and have no history of smoking, chances are you have a benign condition that can be treated.
The most definitive way to get rid of your brown phlegm is to resolve the underlying condition that is causing your symptom in the first place.
If the cause of your lung damage is primarily due to smoking, your healthcare provider will suggest that you quit immediately. You may notice that your symptoms are getting better in just a matter of days or weeks.
If air pollution or toxic substances are the cause of your lung damage, it may be best for you to move or quit your job, although understandably, this may not be feasible for everyone. Sometimes contaminants in the home (such as mold) can be mitigated if identified.
Antibiotics may be used to treat bacterial pneumonia and lung abscesses. Antivirals may be used in some types of viral infections. Finally, lung cancer is often treated with a combination of surgery, chemotherapy, and radiation.
Complications and Risk Factors Associated With Brown Mucus/Phlegm
Your mucus turns brown because damage to the upper respiratory tract from chronic inflammation mixes mucus with old blood, tar, or debris (or a combination of all three). Inflammation within the lung also leads to an overall increase in mucus production which can cause a chronic cough.
Medical complications associated with the development of brown mucus or phlegm include:
- Lung cancer
- Lung abscess
- Bacterial pneumonia
- Black lung (coal miners’ lung or coal workers’ pneumoconiosis)
- Fungal infections of the lung, such as aspergillosis
- Lung damage due to smoke inhalation from a house fire or wildfire
The following risk factors are associated with an increased risk of upper respiratory lung damage:
- Older age
- History of smoking (especially a history of early smoking before age 45 for 10 or more years)
- Occupational exposure to chemicals toxic to the lungs
- Weakened immune system
Are There Tests to Diagnose the Cause of Brown Mucus/Phlegm?
The tests for diagnosing the cause of your brown mucus will depend on your clinical presentation, medical/smoking history, and physical examination.
- Labs: A complete blood cell count with differential, viral tests (flu and COVID-19), and a basic metabolic panel can help detect underlying infections.
- Imaging: A chest X-ray is a quick, cheap, and effective way to identify the presence of infection (pneumonia or abscess) in the lungs. Computed tomography (CT) scans of the lungs can provide a more detailed look at the damage, especially by tumors or chronic lung diseases.
- Bronchoscopy: A scope with a camera at the end can look at your lungs and even be used to biopsy (take a sample for analysis) suspicious lesions or masses that may be the cause of your brown phlegm.
- Sputum culture: This test looks for organisms (fungi or bacteria) that may be causing an infection in the lungs.
When to See a Healthcare Provider
If your symptoms do not improve or worsen even after treatment or present with ominous signs such as thick or smelly discharge, fever, shortness of breath, extreme fatigue, or unexplained weight loss, seek immediate medical attention.
Consulting a healthcare provider may help you to determine new or better treatments or help you determine if there is a need for more imaging and a bronchoscopy to figure out the precise cause of your brown sputum.
Summary
Brown mucus is a less common form of phlegm that is caused by a variety of conditions, ranging from smoking and air pollution to chronic lung disease and bacterial or viral infections. See a healthcare provider if this symptom persists or is accompanied by other symptoms such as fever, shortness of breath, chest pain, or unexplained weight loss.
A Word From Verywell
Mucus production is important to your health because it protects against infection. It serves the dual role of trapping debris and foreign substances while also keeping your airways moist. Under normal circumstances, mucus is clear and thin, but if it changes color, it may be a sign of underlying disease.
If your mucus has changed color, texture, or volume, worsened despite treatment, or is associated with systemic symptoms like fever or significant weight loss, seek immediate medical attention because this may be a sign of a medical emergency.
Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
- The Ohio State University Wexner Medical Center. What does the color of phlegm mean?
- American Cancer Society. What causes lung cancer?
- Thomson B, Emberson J, Lacey B, et al. Association of smoking initiation and cessation across the life course and cancer mortality: prospective study of 410,000 US adults. JAMA Oncology. 2021;7(12):1901-1903. doi:10.1001/jamaoncol.2021.4949
- Kuhajda I, Zarogoulidis K, Tsirgogianni K, et al. Lung abscess-etiology, diagnostic and treatment options. Annals of Translational Medicine. 2015;3(13):183. doi:10.3978/j.issn.2305-5839.2015.07.08
- Kuhajda I, Zarogoulidis K, Tsirgogianni K, et al. Lung abscess-etiology, diagnostic and treatment options. Ann Transl Med. 2015;3(13):183. doi:10.3978/j.issn.2305-5839.2015.07.08
By Shamard Charles, MD, MPH
Shamard Charles, MD, MPH is a public health physician and journalist. He has held positions with major news networks like NBC reporting on health policy, public health initiatives, diversity in medicine, and new developments in health care research and medical treatments.