Conditions That Affect Your Scalp
The cysts are typically large and smooth, and they may be tender. Sometimes, more than one occurs in one area.
How to Manage Scalp Folliculitis
We include products we think are useful for our readers. If you buy through links on this page, we may earn a small commission Here’s our process.
How we vet brands and products
Healthline only shows you brands and products that we stand behind.
- Evaluate ingredients and composition: Do they have the potential to cause harm?
- Fact-check all health claims: Do they align with the current body of scientific evidence?
- Assess the brand: Does it operate with integrity and adhere to industry best practices?
Folliculitis is a common inflammatory skin condition affecting your hair follicles. It’s usually caused by a fungal or bacterial infection.
The infection occurs when you damage your hair follicles, which are the openings in your skin that hold the roots of your hair. This can affect any part of your body with hair, including your scalp.
The condition isn’t contagious, and you can usually treat it at home. But in some cases, the infection can spread to other follicles and cause scarring or permanent hair loss.
Folliculitis initially causes small, red bumps that look similar to an acne breakout. Over time, it may spread to other follicles and the bumps may get larger and more inflamed.
While it can affect any part of your scalp, it often begins along your hairline.
Other signs and symptoms of scalp folliculitis include:
- clusters of tiny, red bumps on your scalp that may have a white tip
- sores with yellowish-brown scabs
- sores that drain pus
- itching
- burning or stinging sensation
- pain or tenderness
Folliculitis is caused by damage to your hair follicles, which leaves them vulnerable to infection-causing bacteria and fungi.
Many things can damage the hair follicles on your scalp, such as:
- frequently scratching or rubbing your head
- tugging on or twisting your hair
- wearing hairstyles that pull your hair, such as tight ponytails or braids
- frequently wearing hats
- shaving your head
- wearing sports helmets
- using a lot of hair products, which can build up over time
Several things can also increase your risk of developing scalp folliculitis, including:
- having acne or dermatitis
- being a male with coarse or curly hair
- having a weakened immune system due to an underlying condition
- taking certain medications for acne, including steroid creams or antibiotic therapy
You can usually take care of mild cases of folliculitis at home. The most important thing is to stop doing anything that may have caused it in the first place.
For example, if you shave your head frequently, try taking a few weeks off. If your folliculitis clears up, you may want to change your shaving technique.
You can also try:
- Warm compress. Applying a warm compress or warm, damp cloth to your scalp a few times a day can help to soothe your scalp and drain any pus.
- Antibacterial soap. If your scalp folliculitis is located along your hairline, gently wash the skin twice daily with antibacterial soap and dry the area with a clean towel.
- Anti-dandruff shampoo. Washing your scalp with an anti-dandruff shampoo that contains antifungal agents, such as ketoconazole, ciclopirox, or tea tree oil, may be helpful. You can buy anti-dandruff shampoo on Amazon.
- Cortisone cream. A cortisone cream, also available on Amazon, can help to soothe the inflammation and itch of scalp folliculitis.
- Antibiotic ointment. You can also try applying an antibiotic ointment, like Neosporin, to the area to help target bacteria.
- Lukewarm water. Avoid washing your hair or scalp with hot water, which can further irritate your scalp. Stick to lukewarm water instead.
- Washing. Wash any items, such as hats, bedding, or combs, that have come into contact with the affected part of your scalp.
Once your condition has cleared up, be sure to practice proper scalp hygiene. Wash your scalp regularly to avoid a buildup of hair products and oils that can clog or irritate your hair follicles.
If you shave your head with a hand razor, consider switching to an electric razor and using a soothing lotion after each shave.
While folliculitis is often treatable at home, some cases may require a trip to the doctor. Make an appointment if you aren’t noticing any improvement after a few days of home treatment, or if things seem to be getting worse.
You should also see a doctor if:
- sores continue to worsen or spread after two full days of home treatment
- your skin is red or painful around the hair follicles
- you develop a fever of over 100°F (38°C)
- your folliculitis was caused by shaving, but you’re not able to stop shaving
You may need a prescription antifungal cream or oral antibiotic, especially if you have a weakened immune system or have recurring folliculitis.
Folliculitis of the scalp can be uncomfortable, but you can usually manage it at home.
If you aren’t noticing any improvement after a few days, or things seem to be getting worse, make an appointment to see a doctor. You may need a prescription treatment.
Last medically reviewed on February 15, 2019
Conditions That Affect Your Scalp

Psoriasis is a long-lasting condition that causes a dry, itchy buildup of skin cells that may crack and bleed. It makes your skin flake, and you can have it on different parts of your body. About half of all people with it have it on their scalp.

Treatment for Scalp Psoriasis
2/18
Your doctor may give you special shampoo or medication to put directly on your scalp. You also may get pills to help with inflammation and itching. Another treatment option is to shine natural or artificial ultraviolet light on your skin. It can help clear up the painful patches.

Dry Scalp
3/18
It sounds simple, but this can have a big effect. It can itch and flake, and when the skin breaks — from cracking or scratching — bacteria can get in and cause an infection. It’s more common in dry climates, and it’s more likely to happen as you get older. You also can have this issue if you wash your hair too often or use harsh hair products that strip out natural oils.

Treatment for Dry Scalp
4/18
Lifestyle changes can make a difference. You may try washing your hair less often or using a milder shampoo — ask a doctor or pharmacist about what might work best for you. In severe cases, or when the dryness is caused by a treatable condition, your doctor may suggest medication.

Dandruff
5/18
Small pieces of skin can “flake” off your scalp and leave a telltale sprinkling of white on your shoulders. Overly dry — or oily — skin can cause it, as can certain illnesses, like HIV or Parkinson’s disease. It also can be a reaction to certain soaps or shampoos or to a fungus on your scalp.

Treatment for Dandruff
6/18
Your treatment will depend on the cause. For example, if it’s a reaction to certain shampoos, you may simply switch products. Or you can try an over-the-counter dandruff shampoo or rinse to manage it. If it doesn’t go away, talk with your doctor.

Ringworm
7/18
Despite the name, no worms are involved in this condition. It’s a fungus that can infect your skin or scalp and cause itchy, scaly, bald patches on your head. It’s easy to get it from someone else, and it’s common in toddlers and children.

Treatment for Ringworm
8/18
Your doctor may give you drugs that you take by mouth, or special shampoos, rinses, or creams to use on your head. The problem should be completely gone after treatment, as long as you don’t catch it again.

Lice
9/18
They’re tiny insects that live in your hair and feed on blood from your scalp. It sounds terrible, but they’re not dangerous — just contagious, annoying, and itchy! They’re also sometimes hard to get rid of.

Treatment for Lice
10/18
Special shampoos or rinses can kill lice and the eggs they lay. You can get some of these over the counter, but higher-strength ones need to be prescribed by your doctor. Your scalp might itch for a while, even after the lice are gone.

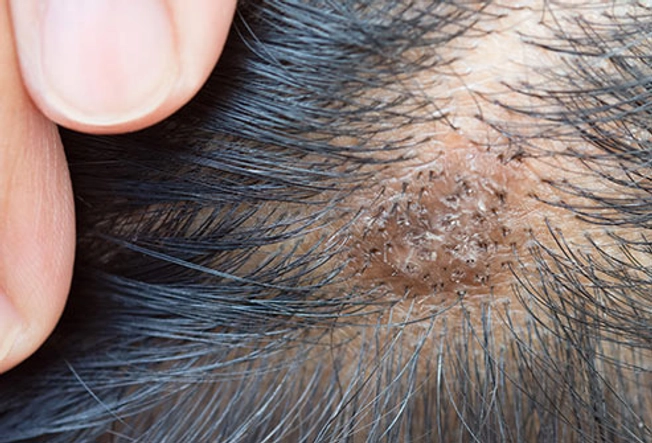
Folliculitis
11/18
This is a common skin condition that happens when hair follicles — the tiny holes where your hair grows — get irritated, usually after a bacterial or fungal infection. Small red or white-headed bumps often show up around the follicles. It can spread and turn into crusty sores that don’t heal fast. In severe cases, it can cause hair loss and scarring.

Treatment for Folliculitis
12/18
It’s treated with medicated creams or shampoos or light therapy. In rare cases, minor surgery may be needed.

Alopecia Areata
13/18
This happens when your immune system, which normally protects your body from invaders like viruses and bacteria, mistakenly attacks your hair follicles. It can lead to hair loss, often in patches.

Treatment for Alopecia Areata
14/18
There’s no cure or any approved drug to help with symptoms, although several medications and surgical procedures look promising for future treatment. Still, your hair might regrow on its own. Medications for hair growth work for some people, but they don’t keep you from getting new patches. It’s important to protect exposed skin — especially on top of your head — from direct sun with hats, scarves, or sunscreen.
Seborrheic Dermatitis
15/18
It causes “scaly” patches of skin and stubborn dandruff and may also affect oily areas of your body, like your face, upper chest, and back. It can be itchy, but it’s not serious.

Treatment for Seborrheic Dermatitis
16/18
It’s a long-term condition, but symptoms can be treated with creams, drugs, and special shampoos.

Cradle Cap
17/18
This is a kind of seborrheic dermatitis that happens to babies. It isn’t painful or itchy like the adult version, but it can be alarming to see the thick, crusty, yellow scales, which aren’t easy to remove, on your baby’s head.

Treatment for Cradle Cap
18/18
It usually clears up on its own. You can wash it daily with a mild shampoo to loosen it. If it’s still there after a few weeks or looks like it’s getting worse, see your baby’s doctor.
Show Sources
IMAGES PROVIDED BY:
1) Farina2000 / Thinkstock
2) diego_cervo / Thinkstock
3) tzahiV / Getty Images
4) Wavebreakmedia / Thinkstock
5) vchal / Thinkstock
6) danr13 / Thinkstock
8) simarik / Thinkstock
9) Centers for Disease Control / Wikimedia
10) AH86 / Thinkstock
11) Nigel Stollery / Medical Images
12) Amélie Benoist Khakurel / Science Source
13) Syldavia / Thinkstock
14) domoyega / Thinkstock
15) wasansos1 / Thinkstock
16) smartstock / Thinkstock
17) russaquarius / Getty Images
18) pookpiik / Thinkstock
Journal of Investigative Dermatology: “A Practical Guide to Scalp Disorders.”
Mayo Clinic: “Cradle Cap,” “Seborrheic Dermatitis,” “Psoriasis,” “Dry Skin,” “Dandruff,” “Ringworm Scalp.”
Nemours Foundation: “Head Lice.”
National Institutes of Health: “Androgenetic Alopecia,” “Questions and Answers about Alopecia Areata.”
What can cause bumps to appear on the scalp?
A variety of health issues can cause bumps to form on the scalp, including folliculitis, acne, head lice, and eczema.
Many causes of bumps in this area are harmless, but receiving a prompt diagnosis and treatment can address any concerns and resolve the issue quickly.
In this article, learn about the health conditions that can lead to bumps on the scalp and when to contact a doctor.
Acne that forms on the scalp can be similar to acne in other areas. A person may have raised bumps, whiteheads, or blackheads, which may be itchy, sore, or tender.
Scalp acne occurs when pores or hair follicles become clogged with dead skin cells or oil. If a person has oily hair or adds certain products to their hair, they might be more susceptible to scalp acne.
Factors that may contribute to scalp acne include:
- a buildup of hair products
- washing the hair infrequently or ineffectively
- sweating in a hat, hood, or beanie
- regular delays between working out and washing the hair
Treatment
If scalp acne develops consistently, wash the hair more thoroughly, and try hypoallergenic hair products.
If the issue persists or gets worse, contact a dermatologist for specific guidance.
Folliculitis is a common infection that develops in hair follicles. It can look similar to acne and causes raised, round, inflamed, and itchy bumps.
The infection develops when bacteria enter damaged follicles, and the underlying cause may involve:
- shaving, plucking, or waxing,
- spending time in an improperly maintained hot tub
- wearing tight clothing or headwear
- taking certain medications
- gaining weight
Treatment
To relieve any pain and help the skin heal, apply a warm compress to the area three or four times a day, for 20 minutes at a time.
If the issue worsens, or the cause is unclear, contact a dermatologist.
Itchiness is the most common symptom of head lice, but bumps on the scalp can also indicate their presence.
Have someone closely examine the area for white eggs or moving lice.
Treatment
Treatment for head lice typically involves using medicated shampoo and combing the area to kill and remove the bugs and their eggs.
There are many types of eczema, and two that can affect the scalp include:
Atopic dermatitis
This type of eczema can develop anywhere on the body, including the scalp.
It causes the skin to become inflamed. On a person with darker skin, the affected areas may become darker, grayish, or purplish. On a person with lighter skin, the areas may redden.
In children, it typically affects the hands, backs of the knees, insides of the elbows, scalp, and face.
Seborrheic dermatitis
Adults with this chronic form of eczema on the scalp may notice color changes such as redness, as well as swelling and greasy scaling.
Beyond the scalp, seborrheic dermatitis can affect the:
- nose, and sometimes just the sides
- upper back
- eyebrows
- armpits
- groin
Treatment
For eczema on the scalp, try medicated shampoos, creams, or ointments.
Scalp psoriasis is a common issue that causes inflamed, sometimes thickened patches of skin covered with silvery-white scales.
Treatment
A combination of care strategies, medicated shampoos, and topical ointments can help.
Contact dermatitis occurs when the skin comes into contact with an allergen or irritant.
When this issue develops on the scalp, hair products containing fragrances or specific chemicals may be responsible.
When the scalp reacts to an irritant or allergen, such as a chemical, it can cause itchiness, a burning sensation, and sometimes blistering.
The reaction can occur within minutes of contact with the irritant.
Treatment
It is important to avoid further contact with products that may be responsible. Also, a doctor may prescribe topical steroids.
These fluid-filled cysts most commonly develop on the scalp. They form in the hair follicles and contain excess keratin, a protein that occurs in the hair, nails, and skin.
The cysts are typically large and smooth, and they may be tender. Sometimes, more than one occurs in one area.
Treatment
Pilar cysts typically go away on their own. To reduce the swelling and any tenderness, try applying a warm, clean washcloth to the area.
If a cyst becomes infected, a doctor may prescribe antibiotics. Also, a doctor may recommend the surgical removal of a cyst.
Hives are a rash consisting of itchy, raised bumps. The rash forms as part of an allergic response, and it can affect any part of the body, including the scalp.
Treatment
Hives usually go away on their own within a few days. However, a doctor can prescribe antihistamines or corticosteroids.
Ringworm is a fungal infection of the skin, and it can form on the scalp. Healthcare professionals may refer to this as tinea capitis.
- itchy skin
- a ring-shaped rash
- inflamed, scaly, cracked skin
- hair loss
Tinea capitis is more common in children than adults.
Treatment
Creams, powders, and lotions do not work for ringworm on the scalp. Instead, a doctor prescribes an oral antifungal medication that a person must take for 1–3 months.
Melanomas can appear on the scalp, as can:
- Squamous cell carcinoma: These lumps can be flesh-colored with varying degrees of scaling, crusting, ulceration, and thickening of the skin.
- Basal cell carcinoma: This type of cancer can cause a smooth, pearly bump to form.
- Merkel cell carcinoma: This rare form of skin cancer can appear as a raised, red or violet patch of skin that is fast-growing, painless, and firm.
Unlike the other bumps or blemishes described above, lumps caused by skin cancer continue to change shape and size.
Treatment
If any bumps on the scalp may indicate cancer, contact a dermatologist immediately.
After making a diagnosis, the doctor will describe the treatments, including surgical and nonsurgical options.
A person can treat most of the health issues that cause bumps on the scalp at home, with care strategies, such as using warm compresses or switching shampoos, and over-the-counter medications.
However, contact a healthcare provider about any unusual growths or symptoms of ringworm or atopic dermatitis.
Also, if any scalp issue persists or worsens, consult a dermatologist.
Bumps on the scalp can result from a variety of health issues, such as acne, eczema, psoriasis, pilar cysts, hives, or ringworm.
Some causes of bumps, such as skin cancer, require urgent medical attention. But often, a person can address the issue at home.
If any lump, bump, or blemish on the scalp is concerning, or if home care is ineffective, contact a dermatologist or another healthcare professional.
Last medically reviewed on November 29, 2020
- Dermatology
- Atopic Dermatitis / Eczema
- Melanoma / Skin Cancer
How we reviewed this article:
Medical News Today has strict sourcing guidelines and draws only from peer-reviewed studies, academic research institutions, and medical journals and associations. We avoid using tertiary references. We link primary sources — including studies, scientific references, and statistics — within each article and also list them in the resources section at the bottom of our articles. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- 10 reasons your scalp itches and how to get relief. (n.d.).
https://www.aad.org/public/everyday-care/itchy-skin/itch-relief/relieve-scalp-itch - Acne-like breakouts could be folliculitis. (n.d.).
https://www.aad.org/public/diseases/a-z/folliculitis - Acne: Tips for managing. (n.d.).
https://www.aad.org/public/diseases/acne/skin-care/tips - Al Aboud, D. M., et al. (2020). Pilar cyst.
https://www.ncbi.nlm.nih.gov/books/NBK534209/ - An overview of the different types of eczema. (n.d.).
https://nationaleczema.org/eczema/types-of-eczema/ - Atopic eczema. (2019).
https://www.nhs.uk/conditions/atopic-eczema/ - Contact dermatitis. (n.d.).
https://nationaleczema.org/eczema/types-of-eczema/contact-dermatitis/ - Eczema (atopic dermatitis) treatment. (2017).
https://www.niaid.nih.gov/diseases-conditions/eczema-treatment - Hives. (2018).
https://www.nhs.uk/conditions/hives/ - Howell, J. Y., et al. (2020). Squamous cell skin cancer.
https://www.ncbi.nlm.nih.gov/books/NBK441939/ - Merkel cell carcinoma treatment (PDQ) — patient version. (2020).
https://www.cancer.gov/types/skin/patient/merkel-cell-treatment-pdq - Nakayama, M. et al. (2011). Basal cell carcinoma of the head and neck.
https://www.hindawi.com/journals/jsc/2011/496910/ - Ngan, V., et al. (2014). Scalp folliculitis
https://www.dermnetnz.org/topics/scalp-folliculitis/ - Scalp psoriasis. (2020).
https://www.psoriasis.org/about-psoriasis/specific-locations/scalp
- Stanway, A. (2004). Scalp psoriasis.
https://dermnetnz.org/topics/scalp-psoriasis/ - Symptoms of ringworm infections. (2018).
https://www.cdc.gov/fungal/diseases/ringworm/symptoms.html - Treatment for ringworm. (2019).
https://www.cdc.gov/fungal/diseases/ringworm/treatment.html
Share this article
Medically reviewed by Reema Patel, MPA, PA-C — By Jesse Klein on November 29, 2020
Latest news
Related Coverage
Medically reviewed by Sara Perkins, MD
Medically reviewed by Gerhard Whitworth, RN
Medically reviewed by Katie Mena, MD
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
Medically reviewed by Debra Sullivan, Ph.D., MSN, R.N., CNE, COI
- About Us
- Contact Us
- Terms of Use
- Privacy Policy
- Privacy Settings
- Advertising Policy
© 2004-2023 Healthline Media UK Ltd, Brighton, UK, a Red Ventures Company. All rights reserved. MNT is the registered trade mark of Healthline Media. Any medical information published on this website is not intended as a substitute for informed medical advice and you should not take any action before consulting with a healthcare professional. See additional information.
© 2004-2023 Healthline Media UK Ltd, Brighton, UK, a Red Ventures Company. All rights reserved. MNT is the registered trade mark of Healthline Media. Any medical information published on this website is not intended as a substitute for informed medical advice and you should not take any action before consulting with a healthcare professional. See additional information.






