What the Different Types of Hemorrhoids Look Like
Hemorrhoids have the same or similar symptoms to some other conditions. For that reason, see a healthcare professional if your symptoms continue for longer than a week.
What Are Hemorrhoids?

Hemorrhoids happen when clusters of veins in the lining of your anal canal get swollen and inflamed. By age 50, about half the population has had one or more symptoms, like pain, itching, or bleeding.
What Are They?
2/10
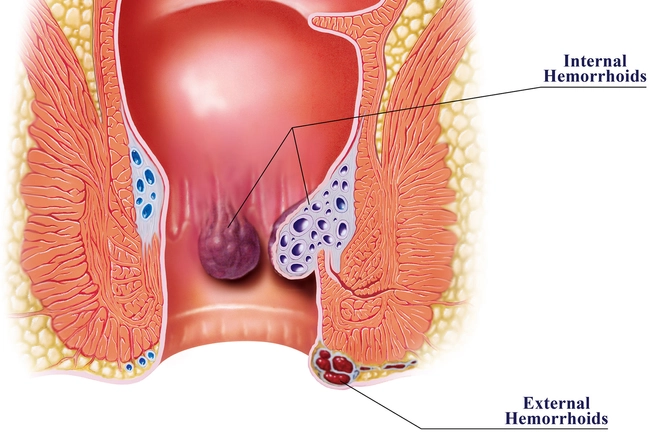
These clumps of veins sometimes stretch when they’re under pressure. They may swell or bulge, kind of like varicose veins. This causes what we call hemorrhoids, or piles. They’re usually not serious, but they can be unpleasant — especially if you keep getting them. Hemorrhoids can form externally, around your anus, or internally, in your lower rectum.

What Causes Them?
3/10
Increased pressure on your lower body can lead to hemorrhoids. This might happen due to:
- Straining during bowel movements
- Constipation or diarrhea
- Being overweight
- Pregnancy or childbirth
- Lifting heavy things
Hemorrhoids are more common as you get older. If your parents had them, you’re more likely to get them, too.
Symptoms
4/10
You might see a little blood on the toilet paper or in the bowl when you go to the bathroom. Your anus could itch or hurt, especially when you sit. Little lumps may form near it. If you notice bleeding, see your doctor. They’ll need to rule out other problems, such as ulcerative colitis, Crohn’s disease, and colon cancer.

How Are They Diagnosed?
5/10
Your doctor will ask about your symptoms and examine you. They may put a gloved finger into your rectum to feel for swollen veins. They also might use an anoscope or a sigmoidoscope, lighted tubes that let them look inside your anal canal.

Prolapse and Thrombosis
6/10
A couple of things can happen that make hemorrhoids more complicated — and painful. When an internal hemorrhoid stretches and pushes outside the anus, that’s called a prolapse. Thrombosis is when a painful blood clot forms in a hemorrhoid. Either problem may heal on its own. (You can even gently nudge a prolapsed hemorrhoid back inside with a finger.) If not, you may need treatment from your doctor.

Food to Prevent and Relieve Them
7/10
Soften your stool and prevent straining on the toilet by eating more fiber. Choose leafy vegetables, fruit, beans, and whole-grain breads and cereals. (Your doctor may also suggest a fiber supplement.) Add fiber to your diet slowly. Too much, too fast can lead to gas and bloating. Drink lots of water to help fiber do its job.

Treatment at Home
8/10
Try nonprescription creams and wipes — or even a small ice pack — to ease pain and swelling. Soak in a warm bath two to three times a day, for 10-15 minutes at a time. Or use a “sitz bath” pan that fits onto your toilet seat. An over-the-counter stool softener can make it easier to go. Drugstore pain relievers like aspirin may ease discomfort.
Treatment by a Doctor
9/10
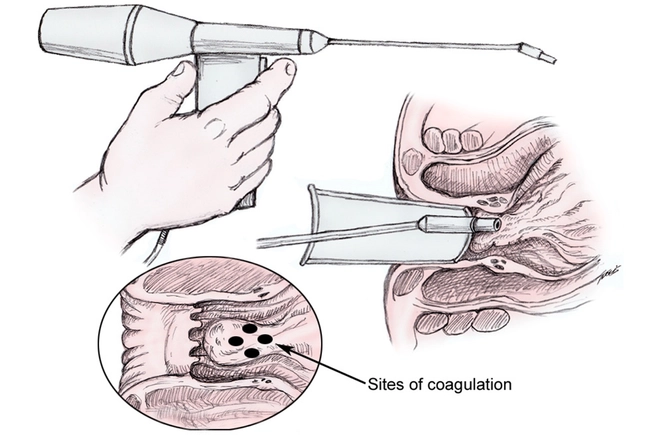
When at-home remedies don’t work, your doctor may put small rubber bands around internal hemorrhoids to cut off the blood supply until they shrink. That’s called ligation. Doctors can use a laser or infrared heat to shrivel internal hemorrhoids, known as coagulation. Or, they can do sclerotherapy by injecting a chemical into the hemorrhoid to break it down.

Surgery
10/10
Most people don’t need surgery for hemorrhoids. But If you have a large external or prolapsed one that won’t go away, a surgeon can cut out the swollen tissues. This operation is called a hemorrhoidectomy. For internal hemorrhoids, you might have hemorrhoid stapling. In this procedure, your doctor uses staples to block blood flow to a hemorrhoid or hold a prolapsed one in place.
Show Sources
IMAGES PROVIDED BY:
1) Thomas Barwick / Getty Images
2) JFalcetti / Getty Images
3) Jose Luis Pelaez Inc / Getty Images
4) penkanya / Getty Images
5) PeopleImages / Getty Images
6) Mikael Häggström . MedicineNet
7) KatarzynaBialasiewicz / Getty Images
8) Sean Justice / Getty Images
9) MedicineNet
10) Portra / Getty Images
American Cancer Society: “Frequently Asked Questions About Colonoscopy and Sigmoidoscopy.”
American Gastroenterological Association: “Living with Hemorrhoids.”
American Society of Colon & Rectal Surgeons: “Hemorrhoids.”
Harvard Health Publications, Harvard Medical School: “Hemorrhoids and what to do about them.”
FamilyDoctor.org: “Hemorrhoids: Causes and Risk Factors.”
UpToDate: “Patient information: Hemorrhoids (Beyond the Basics).”
Cleveland Clinic: “Hemorrhoids.”
Mayo Clinic: “Hemorrhoids.”
What the Different Types of Hemorrhoids Look Like

Hemorrhoids, also called piles, happen when clusters of veins in your rectum or anus get swollen (or dilated). When these veins swell, blood pools inside and causes the veins to expand outward into the membranes around your rectal and anal tissue.
This can become uncomfortable or painful.
There are four types of hemorrhoids:
Most hemorrhoids aren’t a serious medical condition. In fact, you may not even notice them. Less than 5 percent of people who get hemorrhoids have symptoms, and even fewer need treatment.
Hemorrhoids are common. About 1 in 20 Americans are affected by them, according to the National Institutes of Health.
Still, you should see a healthcare professional right away if your hemorrhoids are causing you pain or disrupting your normal activities and bowel movements.
You should also talk with your doctor if they haven’t gone away after a week of treatment at home, or if you’re experiencing bleeding from your rectum.
Hemorrhoids aren’t always visible. But when they expand, they can look like red or blue bumps or lumps.
Here are descriptions of the appearance of the four main types of hemorrhoids:
- Internal. These can’t always be seen because they’re too deep in your anus to be visible. They are protrusions of the wall of your anal canal or rectum. Less-serious internal hemorrhoids are bumps inside, and more serious ones can form a long protrusion.
- Prolapsed. When an internal hemorrhoid swells and elongates to the point where it protrudes out of your anus. Less serious prolapsed hemorrhoids come out of the anus during straining but spontaneously retract when you relax, whereas more serious prolapsed hemorrhoids remain protruding from the anus.
- External. Appear as one or more bumps on and around the anus. You or a doctor can see these from the outside.
- Thrombosed. These are external or internal hemorrhoids in which the blood that’s pooled inside has clotted, which can be painful in external hemorrhoids.
You might have just one hemorrhoid or more than one at a time.
Pictures of the different types of hemorrhoids



Internal hemorrhoids are found inside your rectum. They’re normally not serious and tend to go away on their own.
Sometimes, internal hemorrhoids can swell and stick out of your anus. This is known as a prolapsed hemorrhoid.
There aren’t any nerves that detect pain in your rectum, so you may not always notice internal hemorrhoids. But they can cause symptoms if they grow larger, including:
- pain or discomfort
- itching
- burning
- noticeable lumps or swelling near your anus
Feces traveling through your rectum can also irritate an internal hemorrhoid. This can cause bleeding that you may notice on your toilet tissue.
See your doctor if an internal hemorrhoid causes you a lot of pain or discomfort, or if you experience bleeding from your rectum. Find out more about treatments below.
If you’re having a lot of pain during bowel movements, this may be due to an abscess or fissure in the anus or rectum rather than a hemorrhoid.
A prolapsed hemorrhoid occurs when internal hemorrhoids swell and stick out of your anus. A doctor may assign a grade to a prolapsed hemorrhoid based on how far it protrudes:
- Grade I: Not prolapsed at all.
- Grade II: Prolapsed, but will retract by themselves. These may only prolapse when you put pressure on your anal or rectal area, like by straining when you have a bowel movement, and then return to their normal position afterward.
- Grade III: Prolapsed, and you have to push it back in yourself. These may need to be treated so that they don’t become too painful or infected.
- Grade IV: Prolapsed, and you can’t push it back in without a lot of pain. These will usually need to be treated to prevent pain, discomfort, or further complications.
Prolapsed hemorrhoids look like swollen red lumps or bumps coming out of your anus. You may be able to see them if you use a mirror to examine this area. Prolapsed hemorrhoids may have no other symptom than the protrusion, or they may cause pain or discomfort, itchiness, or burning.
In some cases, you may need surgical treatment to remove or correct a prolapsed hemorrhoid so that they don’t cause you any pain or complications.
External hemorrhoids occur on or around your anus. They’re not always visible but sometimes form lumps on the anal surface.
External hemorrhoids aren’t usually a serious medical issue. But see a healthcare professional if they cause pain or discomfort that affects your daily life.
The symptoms of external hemorrhoids are essentially the same as those of internal ones. But since they’re located on the outside of your rectal area, you may feel more pain or discomfort when you sit down, do physical activities, or have a bowel movement.
They’re also easier to see when they swell, and the bluish color of the dilated veins is visible beneath the anal skin surface.
See your doctor if an external hemorrhoid causes you pain or discomfort.
A thrombosed hemorrhoid contains a blood clot (thrombosis) within the hemorrhoid tissue. They may appear as lumps or swelling around your anus.
Thrombosed hemorrhoids are essentially a complication of a hemorrhoid, in which a blood clot forms.
Blood clots can happen in both internal and external hemorrhoids, and the symptoms may include:
- intense pain and itchiness
- swelling and redness
- bluish color around area of hemorrhoid
See your doctor as soon as possible if you notice increasing pain, itchiness, or inflammation around your rectal and anal area. Thrombosed hemorrhoids need to be treated quickly to prevent complications from a lack of blood supply to your anal or rectal tissue.
Anything that puts pressure or strain on your anus or rectum can cause the veins to dilate. Some common causes and risk factors include:
- having excess weight
- frequently straining during bowel movements
- having diarrhea or constipation
- not having regular bowel movements
- sitting for a long time
- being pregnant or giving birth
- not getting enough fiber in your diet
- using too many laxatives
- getting older, as tissues lose strength and elasticity as you age
Internal hemorrhoids can become prolapsed hemorrhoids if you continue to do any of the things that may have caused your hemorrhoid in the first place.
External hemorrhoids are more likely to become thrombosed, although no specific risk factor is known to cause this.
See a healthcare professional if you start to notice pain and discomfort around your anus, especially when you sit or have a bowel movement.
Seek emergency medical attention if your symptoms worsen suddenly, especially if they’re interfering with your daily activities. Here are symptoms to watch out for:
- feeling extremely itchy around your anus
- burning around your anus
- noticeable lumps or swelling near your anus
- bluish discoloration of your skin near areas of swelling
Your doctor may perform one or more tests to examine the anal or rectal area for hemorrhoids:
- Looking at the anus or rectum. A doctor will likely be able to diagnose an external or prolapsed internal hemorrhoid through a visual examination.
- Doing a digital rectal exam. The doctor will insert a finger covered with a lubricated glove into the anus or rectum to feel for signs of hemorrhoids with the fingers.
- Using an imaging scope. This will help them look at the inside of your rectum to examine for internal hemorrhoids. They’ll usually insert a thin tube with the light on the end into your rectum. Tools used for this diagnosis may include an anoscope or sigmoidoscope.
Hemorrhoids have the same or similar symptoms to some other conditions. For that reason, see a healthcare professional if your symptoms continue for longer than a week.
Some conditions also cause rectal bleeding like hemorrhoids sometimes do. These include:
- colorectal cancer
- ulcers
- gastrointestinal infections
- inflammatory bowel disease (IBD), like ulcerative colitis and Crohn’s disease
But blood from your digestive tract often appears black in your stool unless the bleeding occurs near your rectum and anus. If you’re seeing bright red blood on the toilet paper after you wipe, it’s most likely due to a hemorrhoid or anal fissure.
Anal fissures and anorectal abscesses are the most likely cause of sharp pain while you have a bowel movement, but you might mistake them for a hemorrhoid.
Anal warts are a type of genital wart and can look and feel like a bump on the anus. It’s possible for them to itch and bleed, just like external hemorrhoids.
Because many conditions can be mistaken for hemorrhoids, it’s important to see a healthcare professional for a diagnosis.
Treatment for hemorrhoids depends on the type, degree of prolapse, and severity of your symptoms.
Here are some home remedies to try if your symptoms aren’t too severe:
- Use an over-the-counter hemorrhoid remedy. Hemorrhoid creams or witch hazel solution may help relieve swelling and pain.
- Take pain medications. These include ibuprofen (Advil, Motrin) or acetaminophen (Tylenol), to reduce pain.
- Use a cold compress. An ice pack wrapped in a thin towel can help relive pain and swelling when you apply it to the area.
- Sit in warm water. Do this for about 10 to 15 minutes. You can either fill a bathtub with warm water or use a sitz bath. Some people also use Epsom salts.
In some cases, your hemorrhoids may need to be removed to prevent pain and long-term complications. Some procedures for removal include:
- rubber band ligation
- sclerotherapy
- infrared coagulation
- hemorrhoidectomy
- hemorrhoidopexy
Complications of hemorrhoids are rare. If they do happen, they may include:
- Strangulation. Arteries feeding fresh blood to the hemorrhoid can become blocked, preventing blood supply from reaching the hemorrhoid. This can cause extremely intense and unbearable pain.
- Anemia. If hemorrhoids bleed too much, this can cause fatigue, shortness of breath, headaches, and dizziness due to loss of blood.
- Prolapse. Prolapsed hemorrhoids can cause pain or discomfort when you sit or pass a bowel movement.
- Blood clots. Thrombosis is more likely to be a complication of an external hemorrhoid. Blood clots can cause pain and itching that can become severe.
- Infection. Bacteria can get into hemorrhoids that are bleeding and infect the tissue. Untreated infections can sometimes cause serious complications, like tissue death, abscesses, and fever.
Hemorrhoids can be uncomfortable or even painful, but most of the time, you won’t experience any noticeable symptoms, and complications are very rare.
Internal or external hemorrhoids that don’t prolapse or thrombose are more likely to heal without causing any symptoms or complications. Prolapsed and thrombosed hemorrhoids are much more likely to cause discomfort or increase your risk of complications.
Seek emergency medical attention if your hemorrhoids cause pain and discomfort or if you notice any symptoms like bleeding or prolapse. Hemorrhoids that are treated quickly have a better chance of healing without causing any further complications.
Last medically reviewed on November 29, 2021






