CPAP vs BiPAP – What is the Difference & What Do They Treat
Since PAP machines are only available by prescription, the decision about whether to use BiPAP, CPAP, or another type of PAP therapy must be made by a doctor or sleep specialist.
BiPAP vs. CPAP
We regularly update our articles to include the latest research, expand coverage, and add new information as it becomes available.
Updated December 13, 2022
Both BiPAP and CPAP are types of positive airway pressure (PAP) devices that can be used to treat sleep apnea, a condition marked by paused or shallow breathing during sleep. PAP machines work by sending pressurized air through a hose into a mask worn on the face. This air helps keep the airway open and normalize breathing during sleep.
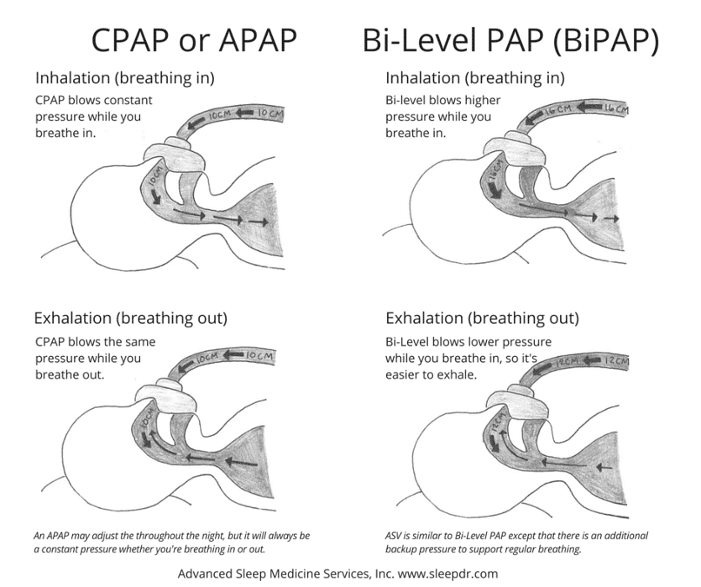
Different PAP machines function somewhat differently. Continuous positive airway pressure (CPAP) machines release a constant level of air pressure. Bilevel positive airway pressure (BiPAP or BPAP) machines release air at two different pressure levels, one for breathing in and one for breathing out.
CPAP is typically the initial treatment for obstructive sleep apnea (OSA), which is the most common type of sleep apnea. However, BiPAP may be prescribed to certain people who have OSA, central sleep apnea, or another sleep-related breathing problem.
For people with sleep apnea, nightly use of a PAP device can improve breathing and sleep. Knowing what distinguishes BiPAP from CPAP machines can help you understand these treatment options and how to make the most of PAP therapy.
What Is BiPAP?
BiPAP stands for bilevel positive airway pressure. A BiPAP machine delivers pressurized air that can keep the airway to the lungs open. This type of machine may be prescribed to people with a sleep-related breathing disorder, like sleep apnea.
In contrast to a CPAP machine, which generally releases air at a single pressure, a BiPAP machine pumps air at two different air pressure levels, one for breathing in and another for breathing out.
How Does BiPAP Work?
BiPAP works by sending pressurized air into the upper airway. This airflow keeps the airway clear of obstruction to prevent lapses in breathing, snoring, and sleep disruptions.
BiPAP treatment is provided using a bedside machine, which is usually small enough to fit inside a shoebox. The machine pressurizes air and pumps it through an attached hose. At the other end of the hose is a mask that is worn over the nose or the nose and mouth. Air flows through the hose and mask and into the upper airway that leads to the lungs.
When the BiPAP machine is turned on, it releases air at two different pressure levels. Inspiratory positive airway pressure (IPAP) refers to the level of air pressure delivered when a sleeper is breathing in. Expiratory positive airway pressure (EPAP) refers to the level of air pressure delivered when a sleeper is breathing out.
A BiPAP machine generally delivers higher air pressure while the sleeper is breathing in and lower air pressure while they are breathing out. The air pressure settings are calibrated carefully to try to make the BiPAP treatment as effective as possible at resolving breathing disruptions.
How Are BiPAP Pressure Levels Determined?
Experts recommend establishing BiPAP settings during a sleep study conducted in a specialized sleep lab. During the study, a technician can closely monitor breathing, oxygen levels, and brain activity. With this data, they can identify which BiPAP pressure levels have the best impact on a specific person’s breathing and sleep quality.
In addition, some BiPAP machines have built-in sensors that are designed to automatically adjust pressure levels to avoid breathing disruptions. These machines can also be used to determine the initial pressure levels. However, experts recommend initially determining optimal pressure levels in a sleep study, instead.
When the auto-adjusting BiPAP technology is used to determine air pressure levels, doctors often closely monitor data from the device and may recommend a follow-up sleep study to confirm that it is working.
Fixed vs. Auto-Adjusting BiPAP
Two types of BiPAP machines are available, and the type of BiPAP machine a sleeper has impacts the air pressure they receive while asleep.
- Fixed BiPAP: In these machines, two fixed air pressure levels — one for breathing in and one for breathing out — are determined by a doctor and programmed into the device. These two levels do not change during the night.
- Auto-adjusting BiPAP: Auto-adjusting BiPAP devices can modify pressure levels in response to a sleeper’s breathing. While these BiPAP machines start with programmed base levels of pressure for breathing in and out, they use sensors to monitor breathing and an algorithm to alter pressure levels as needed.
Because auto-adjusting BiPAP devices are newer, there is limited data showing that they treat sleep apnea and other breathing problems as well as fixed BiPAP devices.
What Are the Different Modes of BiPAP Treatment?
BiPAP machines can be programmed to operate in one of three different modes depending on what is needed to resolve breathing problems.
- Spontaneous mode (S): When in spontaneous mode, the machine delivers pressurized air only when it detects a person beginning to breathe in or out.
- Timed mode (T): In timed mode, the machine pumps air according to a pre-set timer rather than in response to breathing.
- Spontaneous timed mode (S/T): In this mode, the BiPAP machine sends air when the sleeper initiates a breath. However, it also has a timer that triggers the device to pump air if the sleeper doesn’t breathe within a specific amount of time.
What Are the Benefits of BiPAP?
Using PAP therapy can greatly benefit a person with obstructive sleep apnea by reducing daytime sleepiness and improving health and overall quality of life. For people with obstructive sleep apnea, a major benefit of a BiPAP machine is that it may be more comfortable to use than a CPAP machine, because of the lower air pressure level it delivers during exhales.
People who require high levels of air pressure while inhaling in order to resolve their sleep apnea symptoms may especially benefit from using a BiPAP machine. High air pressure might be difficult to tolerate while breathing out. By providing lower pressure during exhalation, a BiPAP machine may encourage nightly use, which is important for treating sleep apnea.
Because a BiPAP machine can be programmed with a timer, BiPAP therapy can also offer benefits to people with health conditions that cause slowed or irregular breathing, including central sleep apnea. In these cases, BiPAP can help regulate breathing and enable better sleep.
What Are the Drawbacks of BiPAP?
When used for obstructive sleep apnea, the main concerns of using a BiPAP machine are the potential for insufficient pressure and higher costs.
By design, a BiPAP device lowers the level of air pressure during exhalation. For some people, it is possible that the pressure will be too low to keep the airway open and successfully treat obstructive sleep apnea.
Another potential drawback is that BiPAP machines can be more expensive than CPAP machines. People whose devices are covered by insurance may not notice a big price difference, but BiPAP therapy may have a larger financial impact on those who have to pay for their machine out of pocket.
How Is BiPAP Different From CPAP?
The key difference between BiPAP and CPAP is that a BiPAP machine provides different air pressure levels for inhalation and exhalation. In contrast, a CPAP machine uses the same amount of air pressure whether the sleeper using the machine is breathing in or out.
In many ways, though, the differences between BiPAP and CPAP machines are growing smaller. Often, contemporary CPAP devices are able to provide more than one level of air pressure. For example, a pressure relief setting on many CPAP devices allows for a minor reduction in air pressure during exhalation.
Is BiPAP Better Than CPAP?
Research studies have found similar results for both CPAP and BiPAP as treatments for obstructive sleep apnea (OSA). For most people with OSA, CPAP is initially recommended because of its simplicity and extensive track record. However, there are circumstances in which BiPAP therapy may be more effective than CPAP.
Who Is BiPAP Best for?
BiPAP machines are typically best for people who have complex sleep-related breathing problems or who have struggled with CPAP therapy.
In people who have obstructive sleep apnea and no other sleep-related breathing problems, BiPAP therapy is most often used in two specific circumstances.
- If high pressure is required: Some sleepers need very high levels of air pressure when they inhale in order to prevent breathing disruptions. A BiPAP machine delivers this higher air pressure, then reduces the pressure level during exhalation.
- If initial CPAP therapy is ineffective: While CPAP helps many people with obstructive sleep apnea, it is not effective for everyone. In addition, some people are bothered by the air pressure provided by the CPAP device when they exhale. In these cases, a switch to BiPAP therapy may help improve breathing during sleep.
BiPAP is also often the best treatment option for people who have complicated breathing disorders, either occurring on their own or alongside obstructive sleep apnea.
For example, BiPAP therapy may be prescribed to people with certain types of central sleep apnea (CSA), which is caused by improper signaling between the brain and the muscles that control breathing. In particular, BiPAP is often recommended for people with CSA tied to health issues that can cause slow or shallow breathing, including:
- Muscular dystrophy
- Obesity hypoventilation syndrome (OHS)
- Chronic obstructive pulmonary disorder (COPD)
- Habitual use of opioid drugs
Since PAP machines are only available by prescription, the decision about whether to use BiPAP, CPAP, or another type of PAP therapy must be made by a doctor or sleep specialist.
How to Make the Most of BiPAP Therapy
To optimize BiPAP therapy, follow any directions provided by your doctor or sleep specialist. For example, a doctor might give guidance about the BiPAP machine’s settings, how often to use the machine, and how to keep it clean and operational. It may also be helpful to review any instructions from the device manufacturer about machine maintenance.
Using a mask that fits well and prevents air leaks is also important for successful PAP therapy. It is normal to try multiple masks before finding the best option, so talk with your doctor if the first mask you are given feels uncomfortable or leaks air.
If you experience any problems with the BiPAP machine, challenges with the mask or other accessories, or persistence of breathing problems or other symptoms, talk with your doctor or sleep specialist about potential solutions.
When to Consider Other Breathing Machines
Although a BiPAP machine can be beneficial in many circumstances, it is sometimes necessary to consider other breathing machines.
For example, if you have obstructive sleep apnea without any other breathing problems, a CPAP machine is likely to be recommended for starting treatment. BiPAP therapy may also not be appropriate for people with central sleep apnea and certain underlying health issues, including some types of heart failure.
If you have already started using a BiPAP machine, you and your doctor may consider another type of breathing machine if you do not see an improvement in your symptoms. Your treatment plan may also be modified if you have had any recent changes to your symptoms or overall health.
Frequently Asked Questions About BiPAP vs. CPAP
How Is BiPAP Different From APAP?
An auto-adjusting positive airway pressure (APAP) device operates similarly to a CPAP device, but modifies the levels of air pressure delivered in response to changes in breathing. Auto-adjusting technology can also be integrated into a BiPAP device, but BiPAPs are frequently prescribed with fixed air pressure settings.
APAP devices are also known as auto-CPAPs, and they may be used as an initial treatment for people with obstructive sleep apnea that do not have other breathing disorders or difficulties. BiPAP machines are generally not first prescribed for obstructive sleep apnea. Instead, BiPAP therapy is often tried when a person with OSA cannot tolerate CPAP or APAP treatment.
Does BiPAP Cost More Than CPAP?
In most cases, a BiPAP machine is more expensive than a CPAP machine. However, the actual out-of-pocket cost depends on your health insurance coverage, including whether you have required copays or deductibles
Is a BiPAP Machine Bigger Than a CPAP?
Although there can be some variation based on the brand and model, most BiPAP and CPAP machines are around the same size. These devices can usually fit on a nightstand to provide easy access during the night
Does a BiPAP Machine Require a Prescription?
A prescription is required to obtain a BiPAP machine or other type of PAP therapy. For this reason, it is important to talk to a doctor or sleep specialist about any concerns related to breathing during sleep.
Is a Pressure Ramp Feature Available on a BiPAP Machine?
Many BiPAP devices include a pressure ramp feature. The ramp function allows for a lower level of air pressure to be delivered during the first 5 to 45 minutes of use after which the device begins to pump at its full prescribed pressure.
How Do You Know if BiPAP Is Working?
The effectiveness of BiPAP therapy is determined by tracking changes in your symptoms and by checking information that is recorded by the device. BiPAP machines collect data about your breathing during sleep, and your doctor can review this data to see how well the BiPAP is improving your breathing problems.
References
- Accessed on August 14, 2022. https://medlineplus.gov/sleepapnea.html
- Accessed on August 14, 2022. https://medlineplus.gov/ency/article/001916.htm
- Accessed on August 14, 2022. https://www.uptodate.com/contents/management-of-obstructive-sleep-apnea-in-adults
- Accessed on August 14, 2022. https://pubmed.ncbi.nlm.nih.gov/30736887/
- Accessed on August 14, 2022. https://www.merckmanuals.com/home/lung-and-airway-disorders/sleep-apnea/sleep-apnea
- Accessed on August 14, 2022. https://www.uptodate.com/contents/mode-selection-for-titration-of-positive-airway-pressure-in-adults-with-obstructive-sleep-apnea
- Accessed on August 14, 2022. https://www.ncbi.nlm.nih.gov/books/NBK459252/
- Accessed on August 14, 2022. https://www.uptodate.com/contents/titration-of-positive-airway-pressure-therapy-for-adults-with-obstructive-sleep-apnea
- Accessed on August 14, 2022. https://www.ninds.nih.gov/health-information/disorders/sleep-apnea
- Accessed on August 14, 2022. https://www.uptodate.com/contents/overview-of-polysomnography-in-adults
- Accessed on August 14, 2022. https://pubmed.ncbi.nlm.nih.gov/30736888/
- Accessed on August 14, 2022. https://www.aastweb.org/blog/bipap-biphasic-positive-airway-pressure-vs.-cpap-therapy
- Accessed on August 14, 2022. https://www.uptodate.com/contents/assessing-and-managing-nonadherence-with-continuous-positive-airway-pressure-cpap-for-adults-with-obstructive-sleep-apnea
- Accessed on August 14, 2022. https://medlineplus.gov/ency/article/003997.htm
- Accessed on August 14, 2022. https://medlineplus.gov/ency/article/002377.htm
- Accessed on August 14, 2022. https://www.uptodate.com/contents/central-sleep-apnea-treatment
- Accessed on August 14, 2022. https://www.uptodate.com/contents/noninvasive-positive-airway-pressure-therapy-for-the-obesity-hypoventilation-syndrome
- Accessed on August 14, 2022. https://www.uptodate.com/contents/nocturnal-ventilatory-support-in-copd
- Accessed on August 14, 2022. https://www.uptodate.com/contents/mode-selection-for-positive-airway-pressure-titration-in-adult-patients-with-central-sleep-apnea-syndromes
- Accessed on August 14, 2022. https://aasm.org/fda-reclassifies-positive-aiway-pressure-class-ii-medical-device/
About The Author
Staff Writer, Product Testing Team
Alison is a health writer with ample experience reading and interpreting academic, peer-reviewed research. Based in San Diego, she is published in the journal PLOS Genetics and the Journal of Biological Chemistry and has been a copywriter for SmartBug media. With a master’s degree in biochemistry from the University of California, Davis, she has nearly a decade of academic research experience in life sciences. She enjoys helping people cut through the noise to understand the bigger picture about sleep and health. Alison likes to stay active with rock climbing, hiking, and walking her dog.
Ask The Sleep Doctor
If you still have questions, email The Sleep Doctor team and we will help you get the answers you need to get the best sleep possible.
CPAP vs BiPAP – What is the Difference & What Do They Treat?


CPAP vs BiPAP – What are the differences and which one do you need?
Sleep apnea is a common sleep disorder in which breathing repeatedly starts and stops. Those with sleep apnea typically feel tired even after a full night’s sleep, followed by morning headaches and irritability.
Sleep apnea affects 3% to 7% of the population, making it one of the most common sleeping disorders out there. While this condition can be a nuisance to the lives of those who have it, there are treatment options that help. Although there are CPAP pillows and other types of sleep medicine, the most common treatment options for sleep apnea include CPAP and BiPAP therapy.
Continuous positive airway pressure (CPAP) is the most common PAP treatment, but bi-level positive airway pressure (BiPAP) works better for others. While they both work in similar ways, there are key differences between the two that determine their effectiveness for your specific condition. So, what is are the differences between CPAP vs BiPAP, and what do they treat?
What Is the Difference Between CPAP and BiPAP Machines?
CPAP and BiPAP machines work in similar ways, but work to treat different types of sleep apnea. There are three types of sleep apnea including obstructive sleep apnea, central sleep apnea, and mixed sleep apnea. Because each of these forms like obstructive sleep apnea and central sleep apnea can have potential impacts on one’s health, it’s important to know the difference between BiPAP vs CPAP machines so you know the best option for your needs.
Differences in CPAP machines and BiPAP machines can be defined as the number of pressure settings each one provides.
– With a continuous positive airway pressure machine (CPAP), patients receive a single pressure of continuous airflow through the face mask.
On the other hand, a BiPAP machine provides two pressure settings:
– one for inhalation and a lower pressure for exhalation. Because of this, many patients with sleep apnea find the BiPAP more comfortable as it’s more customizable for a patient’s needs.
In CPAP and BiPAP machines, pressurized air from the machine is forced down the airway in order to keep it open and free from obstruction, allowing patients to breathe consistently throughout the night. When CPAP therapy cannot be tolerated, that’s when BiPAP therapy comes into play with the two pressure options it provides.
For both CPAP and BiPAP machines, it’s important to keep your mask and tubing clean throughout its use. This can be done using a CPAP cleaner or soap that’s meant to clean the mask.
In order to make the switch from a CPAP machine to a BiPAP machine, patients must seek medical advice from a doctor so they can approve the switch between these pressure machines in order to be covered by insurance.
CPAP Explained

A continuous positive airway pressure machine provides a single pressure of continuous airflow through a full face mask that’s worn while patients sleep to aid their breathing. This pressure that the machine provides is said to both prevent pauses in breathing and snoring, as well used to treat other symptoms that come with having the condition, including:
- Excessive daytime sleepiness
- Insomnia
- Nightmares
- Dry mouth
- Headaches
- Irritability
CPAP machines feature an adjustable pressure setting that ranges from 4 to 20 cm H2O while the user is breathing. Typical medical applications for CPAP machines are used to treat obstructive sleep apnea (OSA) and the use of the machine for preterm infants.
Obstructive sleep apnea has a major impact on cardiovascular function and has been associated with conditions such as congestive heart failure and hypertension. This condition can also overlap with chronic obstructive pulmonary disease (COPD), which can cause long-term chronic health problems.
In order to determine the proper amount of airflow pressure that you need to treat your sleep apnea, talk to your physician so they can evaluate based on your needs. This is typically determined based on your anatomy or weight, or through a sleep study for a more in-depth look at your condition.
Those with sleep apnea typically start treatment with CPAP machines. This condition is often brought up by those who have had heart failure, a stroke, or those who use narcotic pain medications.
BiPAP Explained

Bi-level positive airway pressure therapy (BiPAP) features two air pressure settings that the device is able to alternate between while the patient is breathing at night. With each pressure setting, patients can switch between the higher and lower pressures and inhale with higher pressure and exhale with slightly lower pressure with the full face mask on at night. Most BiPAP machines feature a range of 4 to 25 cm H2O, which is 5 cm higher than CPAP machines.
The two air pressure settings featured in a BiPAP machine include one higher pressure for inhalation called IPAP, and one lower pressure for exhalation, called EPAP. The BiPAP machine itself has up to three settings for the switch between IPAP and EPAP:
The first air pressure setting in a BiPAP machine is a timed switching setting, allowing the user to adjust how long the IPAP and EPAP pressures last. This customizable feature ensures users are able to take the correct number of breaths per minute, so they get the proper treatment for their condition.
Second, the machine has spontaneous switching options that sense the user’s breathing pattern and switch between the IPAP and EPAP air pressure settings. This setting is standard for BiPAP machines, as most users rely on the setting for a restful sleep at night.
Lastly, spontaneous/timed switching combines the first two settings, as timed switching turns on when the device detects that the user’s breathing has dropped below a set number of breaths per minute. This intricate setting also follows the user’s natural breathing patterns.
BiPAP vs CPAP: Which is Best for You?
In order to make the best choice for your condition, we must compare BiPAP vs CPAP therapy to know the difference between the two. Continuous positive airway pressure therapy (CPAP) uses a machine to treat obstructive sleep apnea (OSA) which helps keep the patient’s airway open and helps them breathe better during their sleep at night. Obstructive sleep apnea is the most common form of this condition.
As for BiPAP machines, these devices are often used to treat central sleep apnea (CSA) and complex sleep apnea as well as heart, lung, and neurological disorders that require structured airway support while patients sleep. Treating complex sleep apnea forms with sleep medicine and a BiPAP machine or CPAP machine is crucial in preventing long-term effects on your health.
For the most part, those with sleeping disorders like sleep apnea start off with a CPAP machine for their therapy treatment. When patients first use a CPAP machine with the CPAP mask, there’s typically an adjustment period before you’ll feel comfortable using the device.
If you experience discomfort with CPAP therapy, it can be managed by adjusting the pressure settings, trying different mask types, and experimenting with climate control accessories for those that feature the option.
If you try the continuous positive airway pressure machine for your sleep apnea and you feel the CPAP therapy isn’t right for you, it’s important that you consult a doctor about the possible switch from CPAP to BiPAP therapy. This switch between these pressure machines must be decided on by a doctor and supervised by a sleep specialist in order to verify that the transition is right for your treatment.
If you suspect that you have sleep apnea, contact your primary care doctor. Your doctor may refer you to a sleep specialist to further assess your condition and possibly conduct a sleep study. The machine will then need to be approved by the sleep specialist or doctor for it to be covered by insurance. If left untreated, sleep apnea can increase the risk of serious health problems, making it important that the condition is dealt with as soon as possible.
CPAP vs BiPAP Takeaways (Key Features & Differences):
CPAP
- Continuous Pressure
- Same pressure during exhalation and inhalation
- Used at home
- Usually a simple device
- Needs little monitoring
- Cheaper than BiPAP
BiPAP
- Continuous Pressure
- Pressures are different between inhalation and exhalation (5cmH2O exhalation vs 15cmH2O inhalation)
- Not commonly used at home
- No simple devices
- Pressures need monitoring
- Expensive






