Chemical Burns
First aid
Chemical Burns
Chemical burns are injuries to the skin, eyes, mouth, or internal organs caused by contact with a corrosive substance. They may also be called caustic burns.
Chemical burns can happen in the home, at work, or at school. They can result from an accident or an assault. Although few people in the United States die after contact with chemicals in the home, many substances common in living areas and in storage areas can do serious harm.
Many chemical burns happen accidentally through misuse of products such as those for hair, skin, and nail care. Although injuries do happen at home, the risk of sustaining a chemical burn is much greater in the workplace, especially in businesses and manufacturing plants that use large quantities of chemicals.
Types of Chemical Burns
Chemical burns are classified like other burns based on the amount of damage done:
- Superficial or first-degree burns only affect the outer layer of skin, called the epidermis. The area will be red and painful, but there usually is no permanent damage.
- Partial thickness or second-degree burns extend into the second layer of skin called the dermis. You may have blisters and swelling, and it may leave scars.
- Full thickness or third-degree burns go through the skin and may damage tissue underneath. The area may look black or white. Because nerves are destroyed, you may not feel pain.
Chemical Burn Causes and Risk Factors
Most chemicals that cause burns are either strong acids or bases. A glance at the medical information on the labels of dangerous chemicals confirms the expected toxicity. Commonsense precautions and consumer education can reduce your family’s risk of injury. A variety of household products can cause chemical burns, including:
Major health insurance companies have faced legal trouble over their claim denial practices. In February 2018, the insurance commissioner of California announced plans to investigate Aetna’s coverage denial practices after a former medical director of the insurance company admitted that he never once looked at a patient’s medical records when deciding whether to deny claims over the three years he worked in the position, according to CNN.
- Ammonia
- Battery acid
- Bleach
- Concrete mix
- Drain or toilet bowl cleaners
- Metal cleaners
- Pool chlorinators
- Tooth-whitening products
Infants and older people are most at risk for burns. Chemical burns tend to happen to:
- Young children exploring their environments who get their hands on something dangerous
- People whose jobs put them in contact with chemicals
Chemical Burn Symptoms
Chemical burn of the skin.
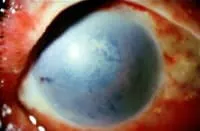
Chemical burn of the eye.
All chemical burns should be considered medical emergencies. If you have a chemical burn of the mouth or throat, call 911 and seek immediate medical attention.
Most chemical burns happen on the face, eyes, arms, and legs. Usually a chemical burn will be relatively small and will require only outpatient treatment. Chemical burns can be deceiving, however. Some agents can cause deep tissue damage not readily apparent when you first look at it.
Signs and symptoms of chemical burns include the following:
- Redness, irritation, or burning at the site of contact
- Pain or numbness at the site of contact
- Formation of blisters or black dead skin at the contact site
- Vision changes if the chemical gets into your eyes
- Cough or shortness of breath
Tissue damage from chemical burns depends on several things, including:
- The strength or concentration of the chemical
- The site of contact (eye, skin, mucous membrane)
- Whether it’s swallowed or inhaled
- Whether or not skin is intact
- How much of the chemical you came into contact with
- Duration of exposure
- How the chemical works
In serious cases, you may develop any of the following:
- Low blood pressure
- Faintness, weakness, dizziness
- Shortness of breath
- Severe cough
- Headache
- Muscle twitching or seizures
- Irregular heartbeat
- Cardiac arrest
- Chemical burns can be very unpredictable. Death from a chemical injury, although rare, can happen.
Emergency Medical Care for Chemical Burns
Any chemical burn can be a legitimate reason to get emergency medical help. Always call 911 if you don’t know how severe the injury is or whether or not the person is medically stable. Also call 911 if you have any concerns about a chemical injury.
Emergency personnel are trained to assess the extent of a chemical burn, begin treatment, and take patients to the hospital.
Emergency workers also may determine the need for more involved decontamination of both you and the accident site prior to going to the hospital. When you contact 911, tell the dispatcher as much of the following information as possible:
- How many people are injured and the location where they are
- How the injury happened
- Whether emergency personnel can reach the victims or whether the victims are trapped
- Name, strength, and volume or quantity of the chemical causing the burn (Give a container of the chemical to emergency personnel, if possible.)
- Length of time of contact with the chemical
Always seek emergency care for any burn that is larger than 3 inches in diameter or is very deep. Also seek emergency care for any chemical burns involving the face, eyes, groin, hands, feet, or buttocks or if it is over a joint.
Even if the exposure was very small and you have completed basic first aid, call your doctor to review the injury and the chemical involved and to make sure no further emergency treatment is needed. The doctor can arrange appropriate treatment or will direct you to go to a hospital’s emergency room. If you’re the person with the burn, ask your doctor if you need a tetanus shot.
Chemical Burn Diagnosis
In the emergency room, you can expect the following:
- Initial evaluation and stabilization
- Rapid evaluation of the chemical
- Determination of the extent of injury
- Blood tests and other studies to determine if you should be admitted to the hospital
Most people with chemical burns do not need to be admitted. Most can go home after arranging follow-up care with their doctor. In severe cases, however, they may need to be admitted to a hospital.
Chemical Burn Treatment
As soon as you or your child have contact with a dangerous chemical, begin basic first aid. Call Poison Control at 800-222-1222 if you do not know whether the chemical is toxic.
Immediately call 911 if you have a severe injury, any shortness of breath, chest pain, dizziness, or other symptoms throughout your body. If you are aiding an injured person with these symptoms, lay the person down and immediately call 911.
First aid
- Remove yourself or the person with the burn from the accident area.
- Remove any contaminated clothing.
- Wash the injured area to dilute or remove the substance, using large volumes of water. Wash for at least 20 minutes, taking care not to allow runoff to contact unaffected parts of your body. Gently brush away any solid materials, again avoiding unaffected body surfaces.
- Especially wash away any chemical in your or the person’s eye. Sometimes the best way to get large amounts of water to your eye is to step into the shower.
Medical treatment
- IV fluids may be needed to normalize blood pressure and heart rate.
- The IV access may also be used for any medications needed to treat pain or protect against infection.
- Decontamination will begin (likely water irrigation).
- You will be given any antidote to counteract the chemical, if appropriate.
- Antibiotics often are not needed for minor chemical burns.
- Wounds will be cleaned and bandaged with medicated creams and sterile wraps as needed.
- Consultation with other medical specialists may be done.
- Pain from a burn can often be severe. Adequate pain control will be addressed by your doctor.
- If there is any indication of breathing problems, a breathing tube may be placed in your airway to help.
- If needed, a tetanus booster will be given.
- Itching as a burn heals can be a serious problem. You may need special medication to soothe it.
- For severe burns, you may need surgery. In a process called skin grafting, a piece of healthy skin from somewhere else on your body or from a donor can be transplanted to replace the damaged skin.
- Cosmetic or reconstructive surgery may be needed to deal with scarring.
- Physical and occupational therapy can keep scars from limiting your range of motion.
- Counseling and support groups can help with emotional issues caused by trauma from the injury or disfigurement.
Chemical Burn Follow-Up
After leaving the emergency department, call your doctor within 24 hours to arrange follow-up care. Call sooner if any new problems or concerns arise.
Chemical Burn Complications
Serious chemical burns can cause long-term complications:
- Many people have pain and scarring.
- Burns in the eye can lead to blindness.
- Swallowing harmful chemicals can lead to problems in your gastrointestinal tract, potentially leading to permanent disability.
- Some acid burns can cause the loss of fingers or toes.
- Burns can cause emotional issues including anxiety, depression, and insomnia.
Chemical Burn Prevention
- Secure all chemicals in and out of the home in locked cabinets or out of the reach of children.
- Store chemicals in their original containers.
- Try to use chemicals as little as possible, and don’t let them touch your skin.
- When using chemicals, always follow directions and safety precautions on the label provided by the manufacturer.
- Make sure your work area is well ventilated.
- Wear safety clothing and eye protection, and remember, safety first!
Chemical Burn Outlook
Most chemical burns are minor and can be treated without causing long-term problems. Some burns, however, cause significant scarring or other medical complications.
Show Sources
eMedicineHealth: “Chemical Burns.”
Mayo Clinic: “Chemical burns: First aid,” “Burns.”
Merck Manual: “Chemical Burns,” ”Burns.”
StatPearls: “Chemical Burns.”
Journal of Surgery: “Caustic burn caused by intradermal self administration of muriatic acid for suicidal attempt: optimal wound healing and functional recovery with a non surgical treatment.”
Johns Hopkins Medicine: “Burns and Wounds.”
American Dental Association: “Tooth Whitening/Bleaching: Treatment Considerations for Dentists and Their Patients.”
International Journal of Molecular Science: “Post-Burn Pruritis.”
National Health Service: “Acid and chemical burns.”
New York Presbyterian/Weill Cornell Medical Center: “Burn Safety and Prevention.”
Department of Health and Human Services: “Effects of Skin Contact with Chemicals.”
Chemical Burns
Chemical burns can happen if you come into contact with a harsh substance such as bleach, battery acid or disinfectants. People who work with chemicals for their jobs are more at risk of chemical burns. Young children are also at risk, since they may accidentally touch or swallow household chemicals.
- Appointments 216.444.5725
- Appointments & Locations
- Request an Appointment
Overview
What is a chemical burn?
A chemical burn is damage to tissue on your body due to a harsh or corrosive substance. You can get chemical burns on your skin, eyes or inside of your body. Most chemical burns are the result of accidentally spilling a chemical on yourself. But it’s also possible to swallow chemicals or get exposed to them in other ways.
Chemical burns range from mild to severe. Mild chemical burns usually heal quickly, but severe chemical burns can cause permanent tissue damage, scarring or death. Chemical burns require immediate medical treatment.
Who’s at risk for chemical burns?
Anyone who works with chemicals is at risk for chemical burns, including:
- Construction workers.
- Factory workers.
- Farmers.
- Laboratory technicians.
- Mechanics.
- Military personnel.
- Plumbers.
It’s important to note that children (especially toddlers) are at a high risk for burns caused by household chemical products. They may accidentally touch or swallow detergents, bleach or cleaning products.
How common are chemical burns?
Between 2005 and 2014, about 3% of all adults admitted to burn centers in the U.S. had chemical burns. One study shows that, over a 17-year period, about 40,000 children (or 2,300 children per year) were admitted to the emergency department with a chemical burn from a household cleaning product.
Symptoms and Causes
What causes chemical burns?
When harsh chemicals come into contact with your skin, eyes or any tissue in your body, they can destroy cells. The damage may go past the superficial layers of skin or tissue and cause deep damage. Chemical burns can be far more serious than thermal (heat) burns. Chemicals often stay on your skin for long periods of time, eating away at your tissue.
There are a lot of substances that can cause chemical burns. Some of the most common include:
- Battery acid.
- Bleach.
- Detergents.
- Drain cleaners.
- Fertilizers.
- Hair relaxers.
- Metal cleaners and rust removers.
- Paint removers.
- Pesticides.
- Sanitizers and disinfectants.
- Swimming pool chemicals.
- Toilet bowl cleaners.
- Wet cement.
What are the symptoms of chemical burns?
Chemical burns on your skin may cause:
- Blisters or scabs.
- Cracked, dry skin.
- Pain.
- Peeling skin.
- Redness.
- Skin discoloration.
- Swelling.
Chemical burns in your eyes may cause:
- Blurry vision.
- Eyelid swelling.
- Pain.
- Redness.
- Stinging or burning.
- Watery eyes.
- Blindness (in severe cases).
Chemical burns from ingestion (swallowing) may cause:
- Chest pain.
- Cough.
- Difficulty speaking (dysphonia).
- Drooling.
- Hoarseness.
- Low blood pressure (hypotension).
- Nausea and vomiting, or vomiting blood.
- Pain in your mouth or throat (especially when swallowing).
- Perforations (holes) in your stomach, esophagus (the tube connecting your stomach and throat) or cornea (the outermost lens of your eye).
- Shortness of breath (dyspnea).
- Upper airway swelling (edema).
Diagnosis and Tests
How are chemical burns diagnosed?
Your healthcare provider can usually diagnose chemical burns on your skin by examining the size, depth and other characteristics of the burn. They may also use other tests to diagnose burns on your skin or in your eyes or from swallowing a chemical, including:
- Blood tests: Swallowing chemicals can affect how your organs work. You can also absorb chemicals in your body through your skin or eye burns. Your healthcare provider may do a complete blood count (CBC) and other lab tests to check your kidney, liver, lung and metabolic function for any type of chemical burn.
- Endoscopy: If you swallow a chemical, you may need an endoscopic evaluation. During an upper endoscopy, your healthcare provider uses a thin, flexible tube with a video camera on one end (endoscope). They guide the tube into your mouth and down your esophagus. Pictures of your throat, esophagus and stomach appear on a video monitor. They can check for burn damaged tissue.
- Eye exam: An ophthalmologist or optometrist (eye care specialist) examines chemical burns to your eyes. They’ll likely flush your eyes out with water. Then, they’ll check for signs of vision loss and examine the depth of the burn. They may also put a special dye into your eye to look for areas of damaged tissue.
- Imaging: Imaging exams help identify damage inside of your body from swallowing a chemical, especially perforations in your esophagus or stomach. You might receive a chest X-ray or CT (computed tomography) scan, which can help spot internal tissue damage.
Management and Treatment
How are chemical burns treated?
Chemical burns require immediate treatment. Call 911 and then:
- Remove clothing: Use gloves to protect your hands. Cut away any clothing contaminated with the chemical. You want to prevent it from touching other areas of your body.
- Remove the chemical: Still wearing gloves, brush away any remaining dry traces of the chemical, but don’t wipe the chemical away. Wiping can spread it to other areas of your skin.
- Rinse with water: Rinse the burned area of your skin or eyes with cool water. Continue rinsing for at least half an hour, as chemicals can continue damaging your skin after contact. Try to keep the contaminated water from touching other parts of your skin. Certain chemicals should not be rinsed with water, including carbolic acid or phenol, sulfuric acid, dry powders and metal compounds.
- Drink water: If you swallowed a chemical substance, drink water to dilute it in your stomach. Don’t take anything to make yourself vomit. Vomiting a chemical substance can cause more damage as it comes back up through your esophagus.
Then, get to a hospital. The American Burn Association recommends that anyone with a chemical burn should seek care at a burn center or call the National Poison Control Hotline (1-800-222-1222) immediately for information on treatment. A burn center is a unit of a hospital dedicated to burn treatment. If you go to the emergency department, they may refer you to a burn center.
Once you arrive at the hospital, your healthcare team will:
- Evaluate the severity of your burn.
- Continue rinsing your burn.
- Give you pain relievers if you’re uncomfortable.
- Apply antibiotics to your skin to prevent infection. Or, they’ll give them to you through a vein in your arm.
- Apply a dry dressing or bandage to mild or moderate burns.
If you have a severe burn, you may need surgery to remove the burned portion of your skin. Some people need a skin graft. A surgeon takes healthy skin from elsewhere on your body and attaches it to the burned area. Surgery can also repair perforations in your gastrointestinal tract.
Prevention
Are chemical burns preventable?
Reduce your risk of chemical burns by taking the proper safety precautions:
- Find alternative products to use that aren’t as harsh.
- Keep chemicals stored in their protective containers.
- Know what chemicals you’re working with and their risks.
- Store chemicals in a secure place, not accessible to children.
- Wear protective clothing or equipment such as gloves, goggles and face shields.
Outlook / Prognosis
What’s the prognosis (outlook) for people with chemical burns?
Most mild chemical burns heal without leaving permanent scars. However, long-term effects of severe chemical burns may include:
- Cancers of your skin, stomach or esophagus.
- Esophageal strictures (narrowed esophagus, sometimes due to scarring).
- Perforations (holes) in your stomach, esophagus or cornea.
- Scars.
- Skin discoloration.
- Vision loss.
Living With
When should I contact my doctor about a chemical burn?
Seek help right away for any type of chemical burn. If you have a burn that’s healing, contact your doctor if the burn:
- Causes severe pain.
- Has yellow or green discharge.
- Is getting worse.
- Looks infected.
What questions should I ask my doctor?
You may want to ask your healthcare provider:
- Are there any risks of long-term complications from a chemical burn?
- How can I reduce the risk of infection and scarring as the chemical burn heals?
- How severe is the chemical burn?
- How can I reduce my risk of getting a chemical burn in the future?
A note from Cleveland Clinic
Chemical burns can happen if you work with chemicals or other harsh substances for your job. People, especially children, can also get chemical burns if they accidentally touch or swallow certain household chemicals. You should seek medical attention from your healthcare provider for any chemical burn, even if it seems mild. Unlike heat burns, chemical burns can continue causing tissue damage even after you come into contact with them. Immediate treatment is essential to prevent scarring or complications.
Chemical and Acid Burns
Christina Donnelly is a freelance writer and editor who has extensively covered health and science content. She currently works at Anthem Health as a content lead.
Updated on February 28, 2022
Michael Menna, DO, is a board-certified, active attending emergency medicine physician at White Plains Hospital in White Plains, New York.
Table of Contents
Table of Contents
Chemical burns—otherwise known as caustic burns—occur when the skin comes into contact with an acid, base, alkali, detergent, or solvent, or the fumes produced by these corrosive materials. They most commonly affect the eyes, face, arms, and legs, but can cause serious damage to the mouth and throat if a corrosive material is ingested.
Fortunately, most chemical burns don’t do major damage to the skin. In fact, many are caused by common household or workplace materials and can be treated in outpatient settings—only about 5 percent of patients seeking emergency medical care for a chemical burn are admitted to the hospital. Highly caustic materials, however, can hurt deep layers of tissue, and the damage isn’t always immediately apparent.
Because the materials that cause chemical burns are so prevalent in homes, schools, and workplaces, it’s important to know what to do if you, a loved one, or a coworker come into contact with caustic materials.
Symptoms of Chemical Burns
The symptoms of a chemical burn depend on a few basic but important factors:
- What substance caused the chemical burn
- Where the substance came into contact with living tissue
- How long the tissue was exposed to the corrosive substance
- Whether the substance was inhaled or ingested
Household bleach coming into contact with your skin, for example, will have a much different effect than bleach coming into contact with your eyes.
Although symptoms can vary widely, common signs and symptoms of a chemical burn include:
- Pain, redness, irritation, burning, or numbness at the site of contact
- The development of blisters or dead, blackened skin at the site of contact
- Blurry vision or total loss of vision if the materials came into contact with the eyes
- Coughing, wheezing, and shortness of breath if the substance was inhaled or ingested
In very severe chemical burns or if a corrosive substance was swallowed, you may experience symptoms like:
- Weakness, dizziness, or fainting
- Headache
- Muscle spasms or seizures
- Low blood pressure, irregular heartbeat, or even cardiac arrest
If you, a loved one, or a coworker comes into contact with a corrosive substance, seek medical care immediately. Even if the exposure seems minor—if a household cleaner splashes on your arms, for example—it’s a good idea to call your healthcare provider or Poison Control Center to determine whether emergency treatment is needed.
If the caustic substance is ingested or if the chemical burn is very deep, more than 3 inches in diameter, or affects the eyes, face, groin, buttocks, or a joint, seek emergency medical care.
Causes
Chemical burns are most commonly caused by exposure to acids or bases in the home, workplace, or at school—they can occur in any place where caustic and corrosive materials are handled. Chemical burns can affect anyone, but people who work in manufacturing facilities, children, and older adults are at the highest risk of injury.
Some common products that can cause chemical burns include:
- Everyday household cleaners like bleach, ammonia, and drain or toilet cleaners
- Skin, hair, and nail care products, and teeth whitening kits
- Car batteries
- Pool chlorine and pool cleaning systems
If possible, read the warnings and medical information on the labels of corrosive products before handling. In many cases, consumer education and proper use can prevent a serious medical emergency.
Although most chemical burns are caused by the accidental misuse of a corrosive substance, they can also be used in assaults. Worldwide, attacks with caustic materials are more likely to occur against women.
Diagnosis
Like symptoms of a chemical burn, diagnoses can vary widely. Your healthcare provider will conduct a physical exam to assess the immediate tissue damage caused by the chemical burn, and ask a series of questions to assess any potential damage. Be sure to tell your healthcare provider about the substance that caused the chemical burn, how long it was in contact with the skin, and the affected body parts.
If you have a severe chemical burn, your healthcare provider may conduct a blood test to determine whether or not hospitalization is required.
After a physical exam and interview, the chemical burn will be categorized as:
- A First-Degree or Superficial Burn: These types of burns affect only the epidermis or the outer layer of the skin. Minor discoloration of the skin is a common symptom of a first-degree burn.
- A Second-Degree or Partial Thickness Burn: Affecting the epidermis and dermis (second) layers of the skin, these burns can be very red, inflamed, and painful, and can blister.
- A Third-Degree or Full-Thickness Burn: The most severe, these burns cause extensive damage to the epidermis and dermis, as well as bones, tendons, muscles, and nerve endings.
Your healthcare provider will recommend treatment options based on the category of your chemical burns.
Treatment of Chemical and Acid Burns
Typically, chemical burns do not require hospitalization or specialized treatment.
For a minor chemical burn, basic first aid can alleviate pain and reduce tissue damage. When treating a minor chemical burn, be sure to:
- Remove yourself, your loved one, or your coworker from the accident area.
- Remove any contaminated clothing.
- Flush the affected tissue with water for at least 20 minutes.
- Remove any foreign objects from the affected area, especially the eyes.
After first aid has been administered, most people with chemical burns simply need to talk to their healthcare provider about follow-up care.
If you or the person affected by a chemical burn begins to experience dizziness, wheezing, difficulty breathing, or other severe symptoms, call 911 immediately.
Some treatments for serious chemical burns include:
- IV fluids to regulate heart rate and blood pressure, or IV medications or antibiotics to treat pain or prevent infection
- Antidotes to counteract the effects of the caustic substance
- Professional cleaning and bandaging
- Pain management through an IV or other pain medications
- A tetanus booster to prevent bacterial infections
Chemical burns rarely result in death, but it’s important to take the steps necessary to avoid infection and protect and heal damaged tissues. If you’ve been treated for a chemical burn, be sure to arrange follow-up care with your healthcare provider within 24 hours of sustaining the injury.
A Word From Verywell
Chemical and acid burns can be painful, but the good news is that most can be treated with basic first aid and follow-up care. Whenever you’re handling corrosive or caustic substances, be sure to read any warning labels and use extra care to avoid contact with your skin, eyes, or mouth. Oftentimes, proper consumer education can prevent serious medical emergencies.
Frequently Asked Questions
How should you treat a bleach burn?
You should treat a bleach burn like most other chemical burns – move to a safe area, remove any clothing and accessories covering the burn, and run cool water over it for 20 minutes. If the burn is mild, you can gently apply an aloe gel or cream to it and place a gauze pad over it. It is a good idea to contact a healthcare provider about the bleach burn even after home treatment; this is especially important if it is on the face, eyes, hands, genitals, scalp, across a joint, or if it was ingested.
Should a mild chemical burn be brought to the hospital?
If a mild chemical burn received proper treatment and the substance that caused it has been identified, the burn may not need to be brought to the hospital. However, a healthcare provider should still be notified in case they wish to treat it themselves. Even if the burn appears minor, it can’t hurt to get it checked out. If the chemical burn shows any signs of infection, like swelling, oozing pus, redness, or an onset of fever, it should be brought to your healthcare provider’s attention.
How long does a chemical burn take to heal?
- First-degree burn: Generally heals within three to six days. After one or two days, the skin can lightly peel.
- Second-degree burn: Healing can take over three weeks. This severity of burn affects the skin’s top layer and a portion of the layer beneath it.
- Third-degree and fourth-degree burn: Multiple weeks or months may be needed to heal this burn. Severe burns can require a skin graft, a procedure in which healthy skin is attached to the damaged area to help with skin repair.
Verywell Health uses only high-quality sources, including peer-reviewed studies, to support the facts within our articles. Read our editorial process to learn more about how we fact-check and keep our content accurate, reliable, and trustworthy.
- Nemours KidsHealth. Burns.
- MedlinePlus. Minor Burns – Aftercare.
Additional Reading
- Johns Hopkins Medical Library. Burns.
- Mayo Clinic. Chemical Burns: First Aid.
- Medscape. Chemical Burns.
By Christina Donnelly
Christina Donnelly is a freelance writer and editor who has extensively covered health and science content. She currently works at Anthem Health as a content lead.


:max_bytes(150000):strip_icc()/chemical-burns-symptoms-causes-diagnosis-treatment-4174243-5bb7be3346e0fb002691d776.png)


