Pictures and Facts About STDs
Genital herpes is part of a large family of viruses known as herpesviruses, which can cause a variety of illnesses such as cold sores, chickenpox, and shingles. Genital herpes is most commonly caused by the herpes simplex virus, type 2 (HSV-2), though less often it can result from a genital infection with herpes simplex virus, type 1 (HSV-1).
Can Genital Herpes Be One Bump or Is It Multiple Blisters?

It’s never fun to find an unidentified bump on your body, especially in the genital region. The first worry that springs to mind for many people is genital herpes. But can genital herpes be one bump? Or does it have to be multiple blisters?
In this post, we’ll talk about what genital herpes is, how to identify it, and whether or not it can appear as a single bump.
What Causes Genital Herpes?
Genital herpes is part of a large family of viruses known as herpesviruses, which can cause a variety of illnesses such as cold sores, chickenpox, and shingles. Genital herpes is most commonly caused by the herpes simplex virus, type 2 (HSV-2), though less often it can result from a genital infection with herpes simplex virus, type 1 (HSV-1).
HSV-2 is a sexually transmitted infection with no known cure. Once you contract the virus, it remains in the nerves around your genital area for the rest of your life.
Not everyone who contracts HSV-2 will develop symptoms. When they do, however, the most easily recognizable symptom is the formation of painful, itchy bumps and blisters in the genital area.
Normally, a first outbreak with genital herpes is accompanied by other, more generalized symptoms, including:
- Body aches
- Fatigue
- Fever and chills
- Headache
- Painful urination
- Swollen lymph nodes in the groin and pelvic area
After blisters form, they may take up to four weeks to heal completely. Fortunately, subsequent outbreaks usually heal within three to seven days, although they can recur fairly frequently.
Genital herpes is an extremely common virus. In the United States alone, one out of six people between the ages of 14 and 49 has an HSV-2 infection, according to the Centers for Disease Control.
What Do Genital Herpes Bumps Look Like?
A genital herpes outbreak can appear in the form of a single fluid-filled sore or a small cluster of blisters. These blisters appear around the genitals, inner thighs, and buttocks. Lesions may sometimes form inside the vagina as well.
Herpes blisters may look like small red bumps in the beginning, but they then visibly fill with fluid. Over the course of several days, these fluid-filled blisters burst naturally, releasing their fluid. A brown or yellow crust forms, and the affected skin begins to heal.
Can Genital Herpes Be One Bump?
A genital herpes outbreak usually begins as a small cluster of blisters. While these may eventually look like one blister, it’s unusual for genital herpes to start as one bump.
If you discover a single bump in your genital area, it could have a number of other causes.
Insect Bite
Insect bites can vary in appearance, but they’re usually a single bump. It’s uncommon for insect bites to occur in the groin area because of the clothing that covers the area. But if you’ve spent a significant amount of time outdoors, you may have received a bite from a mosquito, tick, or any other insect.
Unlike genital herpes blisters, very few insect bites become filled with fluid unless they are infected.
Ingrown Hair
Ingrown hairs in the genital area are fairly common, especially for people who shave in the area. Ingrown hairs occur when a hair grows back into the skin and a pimple-like lesion forms around it.
Ingrown hairs don’t cause the other symptoms that come with a first outbreak of genital herpes, like fever, headache, or swollen lymph nodes. They may be painful or itchy, but if they fill up, they typically contain white pus instead of clear fluid and don’t burst on their own.
Pimple
Pimples most commonly appear on the face, neck, and back, and although they can form in the genital region, it’s uncommon.
Pimples usually appear as red bumps and sometimes contain yellow or white pus. They don’t generally leak unless you squeeze them. Genital herpes lesions, on the other hand, fill with clear fluid and burst on their own within a few days.
What To Do Next
If you have a single, isolated bump in your genital area unaccompanied by other symptoms, it’s probably not genital herpes. However, only a laboratory test can tell for sure.
If you suspect genital herpes, it’s important to take steps to identify it, since HSV-2 is a highly contagious virus.
Contact Your Physician or Clinic
Because the only sure way to diagnose genital herpes is with lab tests, you’ll need to contact your primary care physician, gynecologist, or local health department for testing. There are six ways to test for HSV-2:
- Swab culture of the blister
- Polymerase chain reaction (PCR) test
- Antigen detection
- Antibody blood test
- At-home test
- Lumbar puncture (this is not usually necessary)
Avoid Spreading Genital Herpes to Others
Until you’re completely certain that your bump isn’t genital herpes, it’s important to take certain precautions to keep from spreading HSV-2 to sexual partners.
- Avoid sexual contact until you know your diagnosis.
- Keep the area clean and dry.
- Avoid touching the sore.
- Wash your hands immediately after any possible contact with the sore.
- Don’t pick at the sore.

By getting tested as soon as possible, you’ll be able to move forward with assurance. If your single bump isn’t genital herpes, then you can simply care for it appropriately. If it is genital herpes, you can explore the many options for managing this common illness.
Pictures and Facts About STDs

You don’t have to have sex to get an STD. Skin-to-skin contact is enough to spread HPV, the virus family that causes genital warts. Some types cause warts and are usually harmless, but others may lead to cervical or anal cancer. Vaccines can protect against some of the most dangerous types.
Signs: Pink or flesh-colored warts that are raised, flat, or shaped like cauliflower. Often there are no symptoms.

Crabs (Pubic Lice)
2/23
“Crabs” is the common term for lice that set up shop in pubic hair. The term comes from the shape of the tiny parasites, which look very different from head or body lice. The creatures crawl from one person to another during close contact. Pubic lice can be killed with over-the-counter lotions.
Symptoms: Intense itching, tiny eggs attached to pubic hair, or crawling lice.

Scabies
3/23
Scabies is an itchy infestation caused by a tiny mite that burrows into human skin to lay eggs. It is not always an STD, as it can spread through any skin-to-skin contact. But among young adults, the mites are often acquired during sex. Scabies is treated with prescription creams.
Symptoms: Intense itching especially at night and a pimple-like rash. It may take 2-6 weeks for symptoms to appear.

The Clap (Gonorrhea)
4/23
Gonorrhea spreads easily and can lead to infertility in both men and women, if untreated. Antibiotics stop the infection.
Symptoms: Common symptoms are burning during urination and discharge, but often there are no early symptoms. Later, the infection may cause skin rashes or spread to the joints and blood.
In Men: Discharge from the penis, swollen testicles.
In Women: Vaginal discharge, pelvic pain, spotting. Symptoms may be mild and are easily confused with a urinary tract or vaginal infection.

Syphilis
5/23
Most people don’t notice the early symptoms of syphilis. The USPSTF recommends screening for syphilis infection in persons who are at increased risk for infection. Without treatment, it can lead to paralysis, blindness, and death. Syphilis can be cured with antibiotics.
Signs and Symptoms: The first sign is usually a firm, round, painless sore on the genitals or anus. The disease spreads through direct contact with this sore. Later there may be a rash on the soles, palms, or other parts of the body (seen here), as well as swollen glands, fever, hair loss, or fatigue. In the late stage, symptoms come from damage to organs such as the heart, brain, liver, nerves, and eyes.
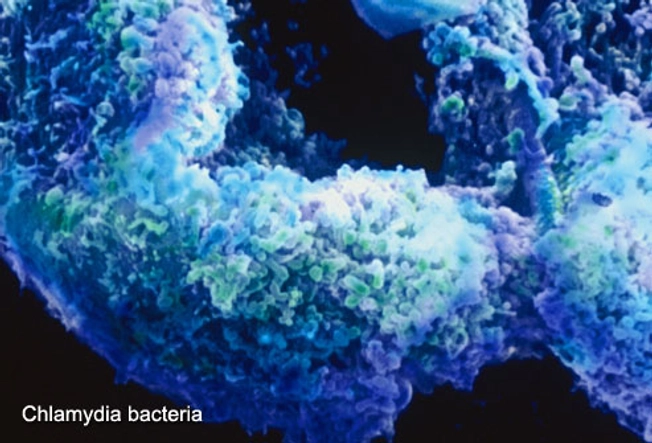
Chlamydia
6/23
Chlamydia is a common STD that can lead to infertility if left untreated. It clears up quickly with antibiotics. But it often goes unnoticed because symptoms are vague or absent. Chlamydia can also infect the rectum and throat.
Symptoms in Men: Burning and itching at the tip of the penis, discharge, painful urination.
Symptoms in Women: Vaginal itching, discharge that may have an odor, pain during sex, painful urination.

Herpes Simplex Virus Type 1
7/23
That painful cold sore you get on your lip every now and then? It’s probably caused by a type of herpes virus called HSV-1. This virus is usually not an STD; it spreads easily among household members or through kissing. But it can be spread to the genitals through oral or genital contact with an infected person. Though there is no cure, drugs can shorten or prevent outbreaks.
Signs and Symptoms: Occasional cold sores or “fever blisters” on the lips. Small blister or sores on the genitals are also possible.
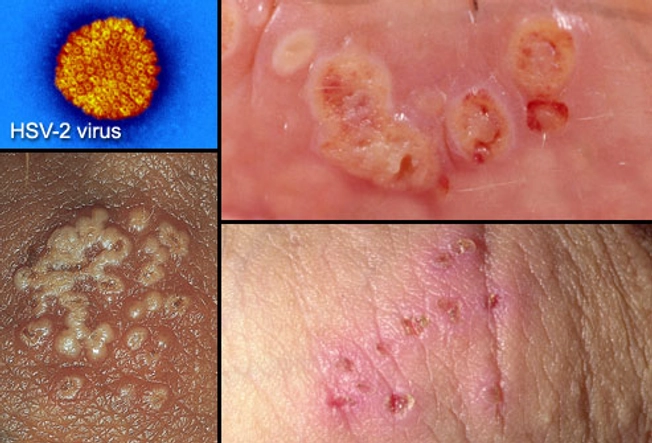
Herpes Simplex Virus Type 2
8/23
Most cases of genital herpes are caused by a virus called HSV-2. It’s highly contagious and can spread through intercourse or direct contact with a herpes sore. As with HSV-1, there is no cure. But antiviral drugs can make outbreaks less frequent and help clear up symptoms more quickly.
Symptoms: Fluid-filled blisters that form painful, crusted sores on the genitals, anus, thighs, or buttocks. Can spread to the lips through oral contact.
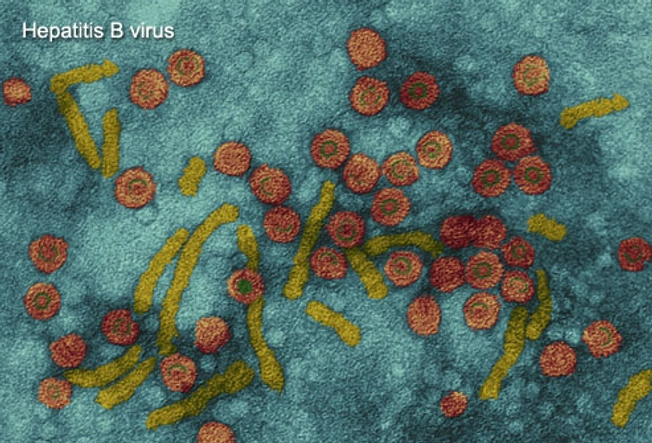
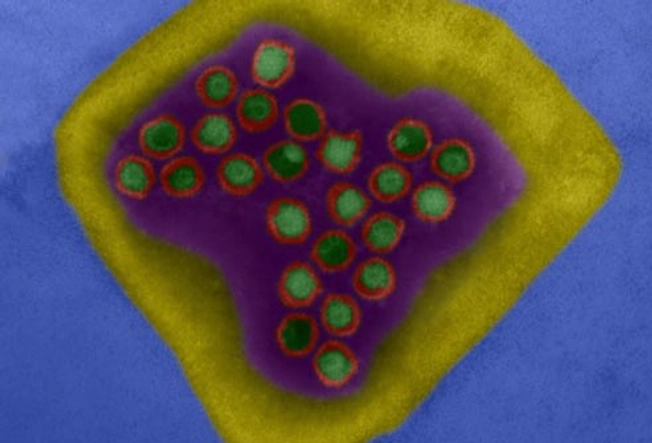
Hepatitis B
9/23
Hepatitis B is a stealthy virus that can cause severe liver damage. It spreads through contact with blood and other body fluids. People can be infected through sex, needle sharing, and at birth, as well as by sharing razors and toothbrushes. There is no cure, but drugs can keep the virus in check. There’s also an effective vaccine to prevent hepatitis B.
Symptoms: People may develop nausea, belly pain, dark urine, fatigue, and a yellowing of the skin or eyes with acute infection. Chronic infection can lead to liver cirrhosis and liver cancer. Many people have no symptoms for years.

HIV/AIDS
10/23
The HIV virus weakens the body’s defense against infections. HIV spreads through unprotected sex, needle sharing, or being born to an infected mother. It may cause no symptoms for years, so a blood test is the best way to learn your status. Timely treatment is important to help prevent serious illnesses.
Early symptoms of HIV Infection: Many have no symptoms, but some people get temporary flu-like symptoms one to two months after infection: swollen glands (seen here), a fever, headaches, and fatigue. Canker sores in the mouth can occur, too.
HIV/AIDS Tests
11/23
Reliable HIV tests can be done in a clinic or at home with the FDA-approved Home Access brand test kit. Anonymous tests use only a number to identify you. One limitation is the “window period” of up to six months after exposure to HIV when these antibody tests sometimes do not find the virus. You can pass HIV to others during that time.
If You Suspect HIV/AIDS: If you’ve been exposed to HIV, starting medications immediately can help prevent infection. If you have the virus, treatments can help prevent HIV from turning into AIDS.

HIV/AIDS Treatment Options
12/23
While there is no cure for HIV, there are medications that can suppress the amount of virus multiplying inside the body. People take a combination of antiviral drugs in hopes of preventing the infection from advancing to AIDS. Additional treatments can help prevent or fight off serious infections, if the immune system has weakened.
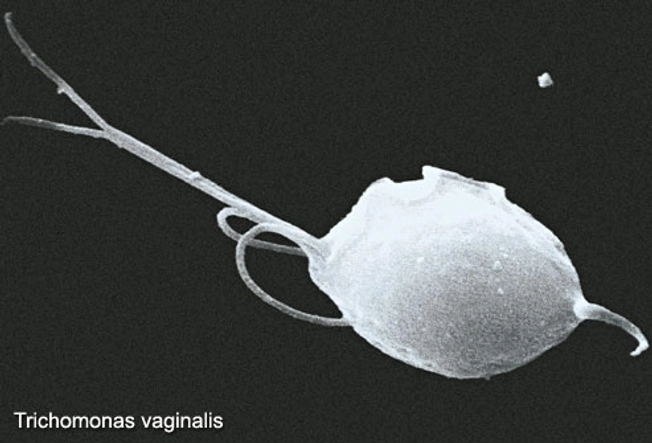
Trichomoniasis
13/23
Trichomoniasis is caused by a parasite that spreads during sexual contact. It can be cured with prescription drugs.
Signs and Symptoms in Men: Most men have no obvious symptoms. Some develop a mild discharge or slight burning during urination.
Signs and Symptoms in Women: Women may develop a yellow-green discharge with a strong odor, vaginal itching, or pain during sex or urination. Symptoms usually begin five to 28 days after acquiring the parasite.
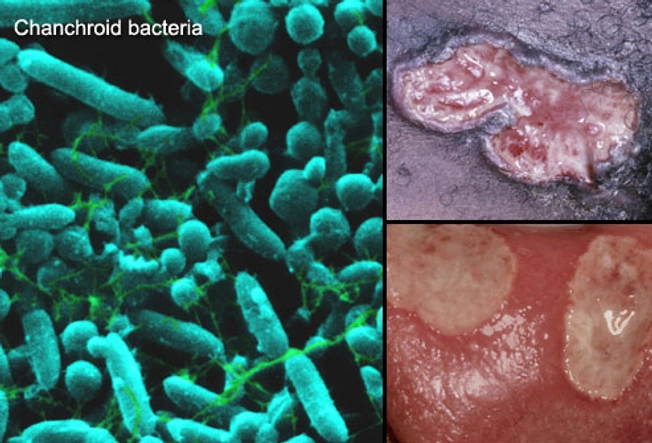
Chancroid
14/23
Chancroid is a bacterial STD that is common in Africa and Asia but rare in the U.S. It causes genital sores that can spread the bacteria from one person to another. Antibiotics can cure the infection.
Symptoms in Men: Painful bumps on the penis that may develop into pus-filled open sores, pain in the genitals and groin.
Symptoms in Women: Painful bumps in the genital area that can develop into open sores, swollen lymph nodes in the groin.

LGV (Lymphogranuloma Venereum)
15/23
LGV is caused by a type of chlamydia that is usually rare in the U.S. But it’s becoming more common in men who have sex with men. Like other forms of chlamydia, it can be cured with antibiotics.
Symptoms: Open sores on the genitals or anus, headache, fever, fatigue, and swollen lymph glands in the groin (seen here). If acquired through anal sex, LGV may cause rectal bleeding or discharge.

Pelvic Inflammatory Disease
16/23
Not an STD itself, pelvic inflammatory disease (PID) is a serious complication of untreated STDs, especially chlamydia and gonorrhea. It happens when bacteria spread to infect the uterus and other female reproductive organs. Prompt treatment is essential to prevent damage to a woman’s fertility.
Signs and Symptoms: Lower abdominal pain, fever, unusual discharge, painful intercourse, painful urination, and spotting. However, there are often no warning signs.

Who’s at Risk for STDs?
17/23
Anyone who is sexually active is at risk for an STD, regardless of gender, race, social class, or sexual orientation. That said, teenagers and young adults acquire STDs more easily than older people. By age 25, half of sexually active adults get an STD. Having multiple sex partners also raises the risk. The CDC has noted that some STDs are on the rise in men who have sex with men, including syphilis and LGV.

Can Virgins Get STDs?
18/23
Yes, they can. Many STDs spread through any type of sexual activity, including skin-to-skin contact and oral sex. This is especially true of STDs that produce genital lesions or sores.

Preventing STDs
19/23
The best ways to avoid getting an STD are to abstain from any sexual contact and be in a monogamous, long-term relationship with an uninfected partner. To reduce the odds of getting STDs:
- Ask your partner if they have an STD.
- Ask partners to be tested before sexual activity.
- Use condoms.
- Avoid sexual activity if your partner has signs of an STD.
- Be aware of symptoms and get regular checkups with your health care provider.

The Limits of Condoms
20/23
While condoms are effective in preventing the spread of some STDs, they are not perfect. Condoms are better at protecting against gonorrhea, chlamydia, HIV, and trichomoniasis. But they offer less protection against herpes, syphilis, and genital warts. These infections can spread through contact with skin lesions that are not covered by a condom. Finally, condoms offer virtually no protection against crabs and scabies.

How to Tell Your Partner
21/23
If you think you have an STD, tell your partner(s) as soon as possible. You may be able to spread the infection even if you have already begun treatment or are using condoms. With some STDs, doctors recommend treating both partners at the same time. This may be a difficult conversation. Some people find it helpful to write a script ahead of time. Be sure to let your partner ask questions and express their feelings.

STDs and Pregnancy
22/23
It is important for pregnant women to be checked for STDs. They can cause women to go into labor too early and may complicate delivery. Many STDs can be passed from mother to baby during pregnancy, childbirth, or after the baby is born. STDs’ effects on babies can include stillbirth, low birth weight, neurologic problems, blindness, liver disease, and serious infection. But there are treatments to minimize these risks. Treatment during pregnancy can cure some STDs and lower the risk of passing the infection to your baby.

Can STDs Come Back?
23/23
Most STD treatments do not protect you from getting the same infection again. A course of drugs may cure gonorrhea, syphilis, chlamydia or trichomoniasis, but a new exposure can start a new infection. If your partner is not treated, you can continue to pass infections back and forth. And if you’re not taking the right precautions to protect yourself, you can be re-infected quickly or even pick up a second STD.
Show Sources
IMAGES PROVIDED BY:
1) Science Source, Dr P. Marazzi, Dr. Harout Tanielian, Biophoto Associates / Photo Researchers Inc.
2) London Scientific Films
3) Dr. P. Marazzi / Photo Researchers, Inc.
4) Juergen Berger / Photo Researchers, Interactive Medical Media LLC , Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology
5) Science Source/Photo Researchers, Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology
6) BSIP/Photo Researchers Inc
7) Interactive Medical Media LLC
8) Interactive Medical Media LLC, Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology, Dr. Harold Fisher/Visuals Unlimited
9) Eye of Science/Photo Researchers Inc
10) Dr. M.A. Ansary / Photo Researchers, Inc., Science Source, Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology
11) Bildagentur RM/Tips Italia
12) Bruce Forester/Photographer’s Choice
13) IMA / Photo Researchers Inc
14) Dr. M.A. Ansary / Photo Researchers, Inc., David M. Phillips / Photo Researchers, Inc, Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatolog
15) Dr. M.A. Ansary / Photo Researchers, Inc.
16) Judith Glick / Phototake
17) Clarissa Leahy/Photographer’s Choice
18) Christoph Martin/Lifesize
19) George Diebold/Photographer’s Choice
20) Michael Winokur/Workbook Stock
21) John Lamb/Stone
22) UHB Trust/Stone
23) Alan Powdrill/Stone
American Social Health Association.
American Social Health Association’s National Herpes Resource Center.
Centers for Disease Control and Prevention web site.
FDA web site.
Fleming, et al. The New England Journal of Medicine, Oct. 16, 1997.
March of Dimes web site.
Merck Manual, 17th edition.
National HIV Testing Resources.
National Institute of Allergy and Infectious Diseases.
National Institutes of Health.
The Nemours Foundation’s Kids Health web site.
U.S. Dept. of Health and Human Services.
Genital Herpes Symptoms, Pictures, and Treatment

You may feel itchy or tingly around your genitals. This is usually followed by painful, small blisters that pop and leave sores that ooze or bleed. Most people notice symptoms within a few weeks after they catch the virus from someone else. The first time it happens, you may also have a fever, headache, or other flu-like feelings. Some people have few or no symptoms.

How You Do — and Don’t — Get Herpes
2/14
You get herpes by having any kind of sex — vaginal, oral, or anal — with someone who’s infected. It’s so common in the U.S. that 1 in every 5 adults has it. Herpes can be spread during oral sex if you or your partner has a cold sore. Because the virus can’t live long outside your body, you can’t catch it from something like a toilet seat or towel.

Worried It’s Herpes?
3/14
Sometimes people mistake a pimple or ingrown hair for herpes. Your doctor can take a small sample from sores by using a swab test. If you don’t have symptoms but think you might have herpes, your doctor can do a blood test. It may take a few days to get your results.
What Causes It?
4/14
Genital herpes usually comes from the virus called herpes simplex-2 (HSV-2). Its cousin, HSV-1, is what gives you cold sores. You can get HSV-2 from someone whether they have symptoms or not.

How Is Herpes Treated?
5/14
Your doctor will prescribe an antiviral medicine. These pills can help you feel better and shorten an outbreak. In the meantime, don’t kiss or have any kind of sex with other people. Even if you don’t have symptoms, you can still spread the disease.

How to Prevent an Outbreak
6/14
Some people only take their medications if they feel the itching and tingling that means an outbreak is coming on — or when sores show up — to stop it from getting worse. Your doctor may suggest you take an antiviral every day if you:
- Have lots of outbreaks
- Want to prevent more outbreaks
- Want to lower the risk of spreading it to your partner

Is There a Cure?
7/14
You can treat herpes, but once you get it, you’ll always have it. When symptoms show up, it’s called having an outbreak. The first is usually the worst. Most people have them on and off for several years, but they get milder and happen less often over time.

How to Avoid Herpes
8/14
As long as you’re sexually active, there’s a chance you could get herpes. You’ll make it a lot less likely if you use a latex or polyurethane condom or dental dam every time, for every activity. The dam or condom only protects the area it covers. If you don’t have herpes, you and your partner should get tested for STDs before sex. If you’re both disease-free and aren’t having sex with other people, you should be safe.

How to Feel Better During an Outbreak
9/14
- Wear loose-fitting clothes and cotton underwear.
- Avoid sun or heat that could cause more blisters.
- Take a warm, soothing bath.
- Don’t use perfumed soaps or douches near your blisters.

What Triggers an Outbreak?
10/14
The herpes virus stays in your body forever, even if you have no symptoms. You may have an outbreak when you’re sick, after you’ve been out in the sun, or when you’re stressed out or tired. If you’re a woman, you could get one when you start your period.

Sex and Herpes
11/14
You still can have sex if you have genital herpes, but you must tell your partner you have the virus. They need to know so they can get tested. Wear a condom any time you have sex. Never have sex during an outbreak.
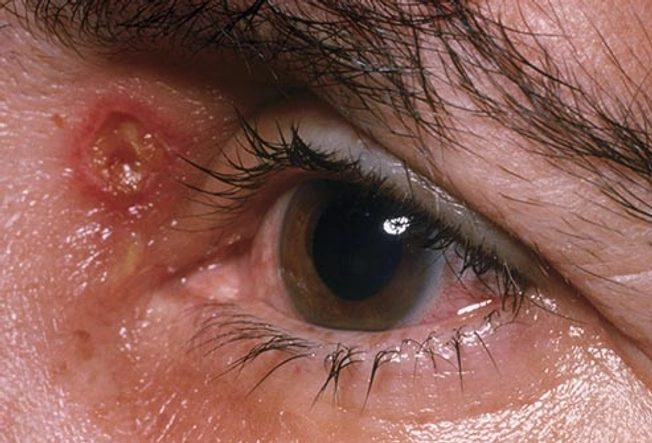
Problems With Herpes
12/14
People often don’t have serious problems from herpes, but there’s a chance of them. Wash your hands often, especially during an outbreak. If you touch a blister and rub your eyes, the infection can spread to your eyes. If your eyes are red, swollen, hurt, or are sensitive to light, see your doctor. Treating it can help prevent serious vision problems.

Herpes and Pregnancy
13/14
If you’re pregnant and have herpes, your doctor may suggest that you have your baby by C-section if you are experiencing an outbreak. Why? During vaginal birth, the herpes virus could spread to your baby, especially if your first outbreak happens around the delivery time. The virus could give your baby rashes, eye problems, or more serious issues. A C-section makes that less likely. Your doctor may also have you take anti-viral medicine starting at about 34 weeks to avoid an outbreak around your due date.

Tips for ‘“The Talk’”
14/14
Getting ready to talk to your partner about herpes? These tips can help you prepare for the conversation. The American Sexual Health Association recommends you pick a time when you won’t be interrupted, plan what you want to say ahead of time, and practice what you’ll say so you feel confident.
Show Sources
IMAGES PROVIDED BY:
(1) Interactive Medical Media LLC, Fitzpatrick’s Color Atlas & Synopsis of Clinical Dermatology, Dr. Harold Fisher
(2) Blend Images
(3) iStock
(4) The Image Bank
(5) Moment Open
(6) Stockbyte
(7) iStock
(8) Photo Alto
(9) Digital Vision
(10) Taxi
(11) Iconica
(12) Photo Researchers / Getty
(13) Monkey Business
(14) Photonica
Brown University Health Education: “Genital Herpes.”
CDC: “Genital Herpes – CDC Fact Sheet.”
Kimberlin, D. Human Herpes Viruses, 2007.
TeensHealth: “Genital Herpes.”
University of Rochester Medical Center: “What You Need to Know About STDs.”
UpToDate.com: “Patient information: Genital herpes (Beyond the Basics).”
WomensHealth.gov: “Genital herpes fact sheet.”
