Heel Spurs and Plantar Fasciitis
Pre-surgical tests or exams are required to identify optimal candidates, and it’s important to observe post-surgical recommendations concerning rest, ice, compression, elevation of the foot, and when to place weight on the operated foot. In some cases, it may be necessary for patients to use bandages, splints, casts, surgical shoes, crutches, or canes after surgery. Possible complications of heel surgery include nerve pain, recurrent heel pain, permanent numbness of the area, infection, and scarring. In addition, with plantar fascia release, there is risk of instability, foot cramps, stress fracture, and tendinitis.
Everything You Need to Know About Heel Spurs
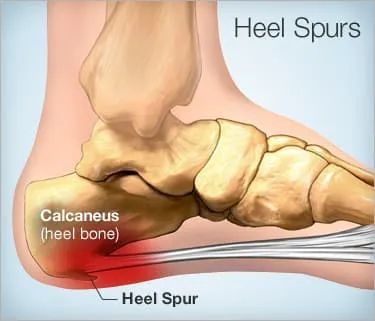
A heel spur is a foot condition that’s created by a bony-like growth, called a calcium deposit, that extends between your heel bone and arch.
Heel spurs often start in the front of and underneath your heel. They eventually affect other parts of your foot. They can get up to half an inch in length. They may not necessarily be visible to the naked eye.
Detecting heel spurs can be challenging. Heel spurs don’t always cause pain, and not all heel pain is related to spurs. Keep reading to learn more about these bony growths and what causes them.
Symptoms of heel spurs may include:
- pain
- inflammation
- swelling at the front of your heel
The affected area may also feel warm to the touch. These symptoms may spread to the arch of your foot. Eventually, a small bony protrusion may be visible.
Some heel spurs may cause no symptoms at all. You may also not see any changes in soft tissues or bones surrounding the heel. Heel spurs are often discovered only through X-rays and other tests done for another foot issue.
Heel spurs are directly caused by long-term muscle and ligament strain. Eventually, this excessive strain stresses the heel bone (calcaneus) causing spurs.
Heel spurs develop over time. They don’t suddenly appear after a workout or a sports event. Heel spurs tend to occur when you ignore early symptoms like heel pain.
Repetitive stress from walking, running, or jumping on hard surfaces is a common cause of heel spurs. They may also develop from wearing shoes that don’t support your foot.
Heel spurs may also be caused by:
- arthritis
- bruising of the heel
- excess body weight
- poorly fitted shoes
- walking gait issues
- wearing flip-flops too often
- worn-out shoes
Many people who have heel spurs also have plantar fasciitis. This painful condition deals with the tough, fibrous tissue that runs between your heel and toes. Having plantar fasciitis increases your risk for eventually developing heel spurs.
Q: What’s the difference between heel spurs and plantar fasciitis?
A: There’s a distinct difference between a heel spur and plantar fasciitis, but the two are closely related. A heel spur is a bony projection that occurs from the bottom of the heel along the course of the plantar fascia. It will vary in size but is usually not larger than half an inch. A heel spur may have no symptoms associated with it. It’s often discovered on an X-ray.
Plantar fasciitis is a painful condition in which there’s an inflammatory process occurring where the plantar fasciitis attaches to the heel. This occurs because of an abnormal force being placed on it. Excess weight, overuse, or wearing shoes without a supporting arch can cause an abnormal force.
As a general rule, plantar fasciitis will subside on its own over a period of time regardless of the treatment. A heel spur will be there permanently, unless surgery is required. Fortunately, surgery is rarely needed.
— William Morrison, MD
Answers represent the opinions of our medical experts. All content is strictly informational and should not be considered medical advice.
It’s difficult for you diagnose a heel spur without medical assistance. This is because the symptoms are similar to other forms of heel pain and foot problems.
You’ll need to see a specialist, such as an orthopedic surgeon or a podiatrist, for a proper diagnosis. They can then detect a heel spur through an X-ray. You can book an appointment with an orthopedist in your area using our Healthline FindCare tool.
Bony protrusions aren’t usually visible to the naked eye. That’s why diagnostic imaging tools are essential if you’re experiencing any unknown causes of foot pain and inflammation.
Before ordering imaging tests, your doctor will conduct a physical examination of your foot to look for any signs of redness or inflammation. Your doctor will also check for any noticeable tenderness on the foot. Tenderness is another indication of a heel spur.
Your podiatrist may also have you do physical tests, such as standing on one foot at a time, as well as taking a brief walk.
Heel spur treatment primarily consists of rest and lifestyle changes. Talk to your doctor about the following treatment options for heel spurs.
Cold compresses
Using ice packs or cold compresses for up to 15 minutes at a time may help relieve heel spur pain by temporarily numbing the area. This method also helps reduce swelling. Cold compresses are preferable over heat packs for heel spurs because heat works better for joint and muscle aches.
Injections of anti-inflammatory medications
For severe pain, your podiatrist may recommend corticosteroid shots. These anti-inflammatory injections help to ease both pain and inflammation throughout the heel and arch of the foot.
Over-the-counter pain medications
Acute, or short-term, pain may be reduced with the help of over-the-counter (OTC) pain medications. These may include acetaminophen (Tylenol), aspirin, or ibuprofen (Advil, Motrin).
Tell your doctor if you’re taking any other medications, such as blood thinners, or if you have any preexisting liver or kidney problems that could prevent you from taking OTC pain relievers.
Physical therapy exercises and stretching exercises
Your podiatrist may recommend physical therapy as a way to learn and practice exercises to prevent long-term pain, especially since anti-inflammatory medications can only be safely taken for a short amount of time.
Heel spur exercises consist of stretching the heel and plantar fascia muscles. Your physical therapist can show you how to do some of the exercises at home. These can be performed at any time of the day, but stretches can be especially helpful at night before bedtime.
Rest
Rest is one of the most recommended treatment measures for both plantar fasciitis and heel spurs.
Not only does rest help alleviate acute pain, but getting off your feet can also prevent your condition from worsening. It’s especially important to rest the feet after long periods of standing and other activities.
In the case of acute pain from a heel spur, your podiatrist may ask you to rest your foot until your symptoms subside. Putting weight on your heel while it’s in pain will likely worsen your condition. It could also lengthen your recovery time.
Orthotic shoe inserts
Orthotic shoe inserts, such as heel pads, can help give you the arch and heel support needed to reduce pain. Heel pads can also prevent further wear and tear. They should be used in addition to proper footwear for all-around foot protection.
Your doctor may recommend surgery when heel spur pain becomes severe and ongoing. This type of surgery involves removing the heel spur. Sometimes it also involves releasing the plantar fascia.
Heel spur surgery not only reduces pain, but it’s also aimed at boosting mobility in the overall foot. Most people who have this type of surgery also have plantar fasciitis. Due to other forms of treatments and therapies available, surgery is not common for heel spurs alone.
Before recommending heel spur surgery, your doctor will determine if you’re a proper candidate by conducting final imaging tests via X-rays and EKGs, as well as blood flow tests to the foot.
It will also take time for you to fully recover from heel spur surgery so that you’re able to put weight on your foot again. The recovery process might include:
- resting your foot and using ice
- compression
- supportive gear
Stretching exercises are good methods of overall body conditioning because they help you work out sore muscles and tight ligaments while also preventing injuries. The same concept applies to heel spur pain management and recovery.
Certain types of stretches can help improve pain and inflammation in your heel and calf areas. These include:
- calf stretches against the wall
- calf stretches on steps
- golf/tennis ball foot rolls
- seated foot flexes
- towel grabs with your toes
Heel Spurs and Plantar Fasciitis
A heel spur is a calcium deposit causing a bony protrusion on the underside of the heel bone. On an X-ray, a heel spur can extend forward by as much as a half-inch. Without visible X-ray evidence, the condition is sometimes known as “heel spur syndrome.”
Although heel spurs are often painless, they can cause heel pain. They are frequently associated with plantar fasciitis, a painful inflammation of the fibrous band of connective tissue (plantar fascia) that runs along the bottom of the foot and connects the heel bone to the ball of the foot.
Treatments for heel spurs and associated conditions include exercise, custom-made orthotics, anti-inflammatory medications, and cortisone injections. If conservative treatments fail, surgery may be necessary.
Causes of Heel Spurs
Heel spurs occur when calcium deposits build up on the underside of the heel bone, a process that usually occurs over a period of many months. Heel spurs are often caused by strains on foot muscles and ligaments, stretching of the plantar fascia, and repeated tearing of the membrane that covers the heel bone. Heel spurs are especially common among athletes whose activities include large amounts of running and jumping.
Risk factors for heel spurs include:
- Walking gait abnormalities,which place excessive stress on the heel bone, ligaments, and nerves near the heel
- Running or jogging, especially on hard surfaces
- Poorly fitted or badly worn shoes, especially those lacking appropriate arch support
- Excess weight and obesity
Other risk factors associated with plantar fasciitis include:
- Increasing age, which decreases plantar fascia flexibility and thins the heel’s protective fat pad
- Diabetes
- Spending most of the day on one’s feet
- Frequent short bursts of physical activity
- Having either flat feet or high arches
Symptoms of Heel Spurs
Heel spurs often cause no symptoms. But heel spurs can be associated with intermittent or chronic pain — especially while walking, jogging, or running — if inflammation develops at the point of the spur formation. In general, the cause of the pain is not the heel spur itself but the soft-tissue injury associated with it.
Many people describe the pain of heel spurs and plantar fasciitis as a knife or pin sticking into the bottom of their feet when they first stand up in the morning — a pain that later turns into a dull ache. They often complain that the sharp pain returns after they stand up after sitting for a prolonged period of time.
Non-Surgical Treatments for Heel Spurs
The heel pain associated with heel spurs and plantar fasciitis may not respond well to rest. If you walk after a night’s sleep, the pain may feel worse as the plantar fascia suddenly elongates, which stretches and pulls on the heel. The pain often decreases the more you walk. But you may feel a recurrence of pain after either prolonged rest or extensive walking.
If you have heel pain that persists for more than one month, consult a health care provider. They may recommend conservative treatments such as:
- Stretching exercises
- Shoe recommendations
- Taping or strapping to rest stressed muscles and tendons
- Shoe inserts or orthotic devices
- Physical therapy
- Night splints
Heel pain may respond to treatment with over-the-counter medications such as acetaminophen (Tylenol), ibuprofen (Advil), or naproxen (Aleve). In many cases, a functional orthotic device can correct the causes of heel and arch pain such as biomechanical imbalances. In some cases, injection with a corticosteroid may be done to relieve inflammation in the area.
Surgery for Heel Spurs
More than 90 percent of people get better with nonsurgical treatments. If conservative treatment fails to treat symptoms of heel spurs after a period of 9 to 12 months, surgery may be necessary to relieve pain and restore mobility. Surgical techniques include:
- Release of the plantar fascia
- Removal of a spur
Pre-surgical tests or exams are required to identify optimal candidates, and it’s important to observe post-surgical recommendations concerning rest, ice, compression, elevation of the foot, and when to place weight on the operated foot. In some cases, it may be necessary for patients to use bandages, splints, casts, surgical shoes, crutches, or canes after surgery. Possible complications of heel surgery include nerve pain, recurrent heel pain, permanent numbness of the area, infection, and scarring. In addition, with plantar fascia release, there is risk of instability, foot cramps, stress fracture, and tendinitis.
Prevention of Heel Spurs
You can prevent heel spurs by wearing well-fitting shoes with shock-absorbent soles, rigid shanks, and supportive heel counters; choosing appropriate shoes for each physical activity; warming up and doing stretching exercises before each activity; and pacing yourself during the activities.
Avoid wearing shoes with excessive wear on the heels and soles. If you are overweight, losing weight may also help prevent heel spurs.
Show Sources
SOURCES:
American Podiatric Medical Association: “Heel Pain,” “General Foot Health.”
American Academy of Podiatric Sports Medicine: “Running and Your Feet.”
American Podiatric Medical Association: “Rearfoot Surgery.”
FamilyDoctor.org: “Plantar Fasciitis: “A Common Cause of Heel Pain.”
Green, D. Podiatry Today, May 2006.
DeLee: DeLee and Drez’s Orthopaedic Sports Medicine, 3rd ed.
The Nemours Foundation.






