Physical Medicine and Rehabilitation
When you have pelvic floor dysfunction, your pelvic muscles can’t relax or work together the way they should. If these muscles can’t relax, only tighten, you may have:
What Is Pelvic Floor Therapy?
Pelvic floor physical therapy is a treatment for problems related to the pelvic floor. This specialized therapy includes exercises that can help relieve symptoms like pain, discomfort, and disruptions to your quality of life.
The Pelvic Floor
Everyone has a pelvic floor. It’s made up of the muscles that support the urinary and reproductive tracts. This group of muscles also controls your bladder and bowels.
In women, the pelvic floor keeps your bladder in place in the front and the vagina and rectum in the back. Your uterus is held in place at the top of the pelvic floor by muscles, tendons, and connective tissue. In men, the pelvic floor helps keep the bowels, bladder, urethra, and rectum in place.
The pelvic floor muscles attach to your tail bone and pubic bone. If the muscles in the pelvic floor are weak or don’t work as they should, this is called pelvic floor dysfunction.
Pelvic Floor Dysfunction
When you have pelvic floor dysfunction, your pelvic muscles can’t relax or work together the way they should. If these muscles can’t relax, only tighten, you may have:
Physician is a high-paying career, and American doctors have some of the highest salaries worldwide, with general practitioners earning an average of $185,000 and surgeons earning $306,000 annually, according to MLive Media Group.
- Constipation
- Peeing frequently
- Trouble controlling your bowels or urine, leading to leaks
- Pain during sex in women
- Erectile dysfunction in men
Sometimes, experts aren’t sure what causes pelvic floor dysfunction. But things that may trigger it include:
- Pelvic surgery
- Aging
- Pregnancy
- Being overweight
- Overuse of the pelvic muscles
- Serious injuries to the pelvic area
Physical Therapy
Pelvic floor physical therapy is a specialized kind of physical therapy to relieve the symptoms of pelvic floor dysfunction and help the muscles work the way they should. This includes several exercises that help your pelvic muscles relax and get stronger.
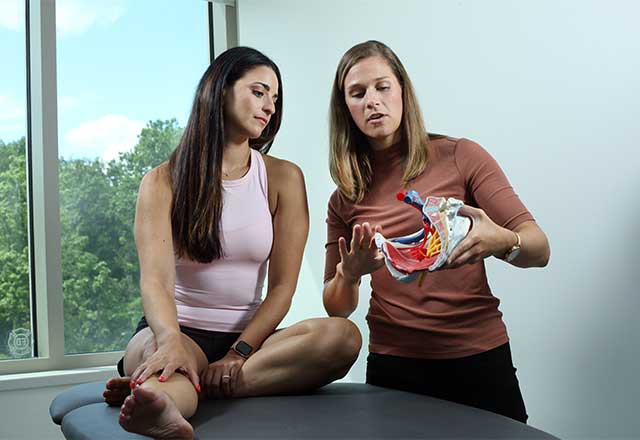
When you begin pelvic floor therapy, a physical therapist (PT) will learn more about your symptoms. Your PT will check your core muscles to see how strong they are, along with how much core endurance you have. Your PT will also have you try certain activities and positions to check the coordination of your pelvic floor muscles.
Your assessment helps your PT make a pelvic floor physical therapy plan that best suits your needs. Your treatment will probably include both internal and external therapy. But they won’t begin internal therapy until you’re ready, because this can be uncomfortable for some people.
The goal of pelvic floor physical therapy is to ease your symptoms so that you can get back to your daily routine. This includes being able to control your bladder better or take part in sports and exercises that you enjoy.
Physical therapy can also relieve the discomfort and pain that women may feel during sex. Some exercises may help them to become more aware of their muscles and have better orgasms.
Techniques and Exercises
Pelvic floor physical therapy can include techniques or exercises like:
Trigger point therapy. This technique puts pressure on a spot on your body, internally or externally, called trigger points. Your doctor or PT may also inject anesthesia into the area.
Kegels.Kegels are a popular exercise for strengthening the pelvic floor muscles by contracting and relaxing them. This exercise can help relieve pain during sex and control incontinence. Your PT can teach you how to do Kegels so that you can get the most out of this exercise.
Electrical stimulation. This technique helps to reduce pelvic pain and muscle spasms. Your PT may do this in the office or teach you how to do it at home with special equipment.
Biofeedback. This technique uses devices to check the contraction of your pelvic floor muscles. Your PT will most likely use biofeedback to see how your exercises are going and to watch for improvement. They may place electrodes on the outside of your body, such as between the vagina or anus. Or they might use an internal probe to measure the tension and relaxation of your pelvic floor muscles. The results are shown on a computer screen, and your PT will discuss them with you.
Show Sources
Beaumont: “Pelvic Floor Physical Therapy.”
Cleveland Clinic: “Pelvic Floor Dysfunction.”
Loma Linda University Health: “Could Pelvic Floor Physical Therapy Help You?”
NAMS: “Yoga, Kegel Exercises, Pelvic Floor Physical Therapy.”
Voices for PFD: “Physical Therapy.”
Pelvic Floor Therapy
At Johns Hopkins, our pelvic health physical therapists are specially trained to evaluate and treat different types of pelvic floor dysfunction, helping you improve your quality of life. We work with patients of all ages and genders, and offer several convenient clinic locations through the Johns Hopkins Rehabilitation Network.
Pelvic Floor Therapy: Why Choose Johns Hopkins
- We offer personalized, one-on-one physical therapy sessions in a private setting tailored to your symptoms and health goals.
- With access to a wide range of therapies and technologies, such as laser therapy, electromyography (EMG) biofeedback, electrical stimulation, and various forms of manual therapy and exercise techniques, we are able to find a combination of treatments that works for you.
- Our team includes several certified women’s health physical therapists, as well as therapists with specialized training in neurology, oncology, pediatrics and other related fields.
- Our therapists work closely with specialists in Ob/Gyn, urogynecology, urology, gastroenterology, oncology, pain medicine and many other disciplines to coordinate your care in and outside Johns Hopkins.
Schedule An Appointment
Schedule by phone
Maryland clinics except Bayview: 443-997-5476
Johns Hopkins Bayview: 410-550-0414 Sibley Memorial Hospital: 202-364-7665
Schedule online through MyChart
Pelvic Floor Symptoms and Conditions We Treat
Our therapists treat a variety of pelvic floor symptoms that could stem from interstitial cystitis, levator ani syndrome, pregnancy and childbirth, surgery, as well as chronic disorders and other age- or trauma-related conditions.
- Bladder problems, including urinary leakage, urinary urgency and/or frequency, difficulty emptying the bladder, urinary retention and pain with bladder filling or emptying.
- Bowel problems, including chronic constipation; difficulty passing a bowel movement and incomplete emptying; increased bowel urgency; fecal leakage of solid stool, gas or mucus; pain with bowel movements.
- Pelvic pain, including pain in the pelvic joints associated with transitions or increased activity level; pain in the tailbone; lower abdomen, lower back, groin, buttock or hip; pain in the genitals.
- Pelvic organ prolapse and the feeling of pelvis pressure or heaviness.
- Sexual dysfunction, including pain with sexual activity (dyspareunia); painful speculum exams or inability to tolerate tampon insertion; erectile dysfunction; decreased or overactive arousal symptoms.
Areas of Specialized Expertise
- Pelvic cancer rehabilitation, including restoring function and managing pain and scar tissue discomfort after surgery and/or pelvic radiation for cervical, uterine or colorectal cancer.
- Pelvic floor issues related to neurologic and neuromuscular disorders, such as multiple sclerosis and spinal cord or nerve injury.
- Pregnancy and postpartum pelvic floor therapy, including treatment of pelvic girdle pain, diastasis recti abdominis (separation of abdominal muscles), Cesarean scar weakness and/or pain, perineal healing postpartum and urinary and bowel leakage.
- Pre- and postoperative care forpelvic surgery, such as hysterectomy, pelvic reconstruction, bladder sling, sacral colpopexy and other procedures.
- Pediatric pelvic floor therapy, including treatment of urinary incontinence (enuresis) and constipation in children.
Pelvic Floor Therapies We Use
Your physical therapist will perform a complete musculoskeletal assessment of the trunk and pelvis, including the pelvic floor musculature, and will work with you to set goals and develop a treatment plan that may include:
- Education regarding pelvic floor and behavioral retraining: making lifestyle changes, such as the way you sit or how much coffee you drink, that may help improve your condition.
- Pelvic floor muscle retraining: exercises to strengthen or relax your pelvic muscles, depending on the cause of your condition.
- Functional dry needling: insertion of thin needles along trigger points to reduce pain and restore normal muscle function.
- Myofascial release: manual stimulation of trigger points in the pelvic floor muscles that radiate pain to other areas.
- Myofascial acoustic compression therapy: the use of focused sound waves to reach deep into fascia and muscles, similar to a deep-tissue massage.
- Soft tissue mobilization to help remodel scar tissue.
- Core strengthening and Pilates: exercises that focus on your posture and core strength and help restore pelvic floor tone and stabilize the lumbar region.
- EMG biofeedback: the use of sensors to gather information about your pelvic muscle activity, which then can be used to help you retrain your muscles with specific exercises.
- Electrical stimulation: the use of mild electrical current to stimulate a muscle to help strengthen it or normalize nerve activity.
- Low-level laser therapy: the use of light (without the heat) to help muscles heal on a cellular level; it can be used on even the most sensitive tissues.
- A home exercise program, often starting after the first visit.
Our Team
Nora Arnold | Physical Therapist
Expertise: pelvic health
Locations: Baltimore and Lutherville
Mary Austin | Therapy Manager, JHH Women’s Health Physical Therapy Residency Director, Physical Therapist
Certifications: Board-Certified Women’s Health Specialist
Expertise: pelvic health
Location: Lutherville
Susan Berger | Physical Therapist
Expertise: falls/balance, orthopedics, pelvic health
Location: Columbia
Holly Brook-Cotton | Physical Therapist Assistant
Certifications: Certified Lymphedema Therapist
Expertise: lymphedema, oncology, pelvic health
Location: Odenton
Karen Dobbs | Physical Therapist
Expertise: oncology, pelvic health
Location: Odenton
Susanne Faux | Physical Therapist
Certifications: Certified Lymphedema Therapist
Expertise: breast cancer, falls/balance, lymphedema, neurologic rehabilitation
Location: Columbia
Rudy Maltez Alvarez | Physical Therapist
Certifications: Certified Dry Needling Specialist
Expertise: orthopedics, pelvic health
Location: Sibley
Lola Oyebefun | Physical Therapist
Expertise: orthopedics, pelvic health
Location: Sibley
Laura Scheufele | Physical Therapist, Clinical Specialist
Certifications: Board-Certified Women’s Health Specialist
Expertise: pelvic health
Location: Baltimore
Madeline Urban | Physical Therapist
Certifications: Board-Certified Women’s Health Specialist
Expertise: pelvic health
Location: Lutherville
Johns Hopkins Physical Medicine and Rehabilitation
- Home
- About Us
- Specialty Areas
- Our Team
- Research
- Education & Training
- COVID-19 Rehabilitation Resources
- Locations