Cervical Spondylosis
When the spinal cord gets injured at C6-C7, pain, weakness, or paralysis may occur in one or more parts of the body below the injured level. Reduction of bowel, bladder, and/or breathing functions may occur in some cases.
Degenerative Disk Disease
Degenerative disk disease occurs when the cushioning in your spine begins to wear away. The condition is most common in older adults. After age 40, most people experience some spinal degeneration. The right treatment can lead to pain relief and increased mobility.
- Appointments & Access
- Contact Us
Overview
What is degenerative disk disease?
Degenerative disk disease is when your spinal disks wear down. Spinal disks are rubbery cushions between your vertebrae (bones in your spinal column). They act as shock absorbers and help you move, bend and twist comfortably. Everyone’s spinal disks degenerate over time and is a normal part of aging.
When the cushions wear away, the bones can start to rub together. This contact can cause pain and other problems, such as:
- Adult scoliosis, where the spine curves.
- Herniated disk, also called a bulged, slipped or ruptured disk.
- Spinal stenosis, when the spaces around your spine narrow.
- Spondylolisthesis, when vertebrae move in and out of place.
How common is intervertebral disk degeneration?
Almost everyone has some disk degeneration after age 40, even if they don’t develop symptoms. It can lead to back pain in about 5% of adults.
Who might get degenerative disk disease?
Degenerative disk disease is most common in older adults. Some factors increase your risk of developing degenerative disk disease, including:
- Acute injuries, such as falling.
- Obesity.
- Biological sex, with women being more likely to experience symptoms.
- Smoking.
- Working a physically demanding job.
Symptoms and Causes
What are the symptoms of degenerative disk disease?
The most common symptoms of degenerative disk disease are neck pain and back pain. You may experience pain that:
- Comes and goes, lasting for weeks or months at a time.
- Leads to numbness or tingling in your arms or legs.
- Radiates down your buttocks and lower back.
- Worsens with sitting, bending or lifting.
What causes degenerative disk disease?
Spinal disks wear down as a normal part of aging. Especially after age 40, most people experience some disk degeneration. However, not everyone experiences pain.
You might have pain if your spinal disks:
- Dry out: Your disks have a soft core that mostly contains water. As you get older, that core naturally loses some water. As a result, disks get thinner and don’t provide as much shock absorption as they used to.
- Tear or crack: Minor injuries can lead to small cracks in your spinal disks. These tears are often near nerves. Tears can be painful, even when they are minor. If the outer wall of your spinal disk cracks open, your disk may bulge out of place, known as a herniated disk, which may compress a spinal nerve.
What does degenerative disk pain feel like?
Degenerative disk pain:
- Can happen in the neck or lower back.
- May extend into the arms and hands or into the butt and legs.
- Can be mild, moderate or severe.
- May start and stop.
- Can get worse after certain activities such as bending, twisting or lifting.
- Can get worse over time.
Diagnosis and Tests
How is degenerative disk disease diagnosed?
To diagnose degenerative disk disease, your healthcare provider may start by asking you about your symptoms. Questions may include:
- When does the pain start?
- Where do you feel pain?
- What activities cause the most pain?
- What activities decrease the pain?
- Did you have an injury or accident that led to pain?
- Do you have other symptoms, such as tingling or numbness?
- How far can you walk?
Your healthcare provider may use imaging scans such as X-ray, CT or MRI. These tests can show your healthcare provider the state and alignment of your disks. Your provider may also conduct a physical exam to check your:
- Nerve function: Your provider may use a reflex hammer to check your reactions. Poor or no reaction could mean you have damaged or compressed nerves.
- Pain levels: Your provider may touch or press on specific areas of your back to measure your pain levels.
- Strength: Muscle weakness or shrinking (atrophy) could mean you have nerve damage or degenerated disks.
Management and Treatment
How is degenerative disk disease treated?
Usually, your healthcare provider will recommend noninvasive treatment options first. Your treatment may include:
- Physical therapy: Participating in strengthening and stretching exercises with a trained healthcare provider.
- Medications: Taking nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxers or steroids.
- Steroid injections: Injecting medicine near your spinal nerves, disk or joints to reduce inflammation and pain.
- Radiofrequency neurotomy: Using electric currents to burn sensory nerves and prevent pain signals from reaching your brain.
Can I treat degenerative disk disease at home?
Some people find pain relief through at-home remedies. At-home treatments may decrease pain for a short time. But they are not a long-term treatment for severely degenerated disks. You may try:
- Exercise: Low-impact activity such as walking or swimming can strengthen back muscles and relieve some pain.
- Hot and cold therapy: Alternating ice packs and heating pads every 10 to 15 minutes up to three to four times per day may reduce soreness and inflammation.
- Stretching: Gentle yoga and stretching throughout the day may improve posture and relieve tension.
Do I need surgery for degenerative disk disease?
Many patients do not need surgery for degenerative disk disease. But if you have tried multiple nonsurgical treatments and have persistent pain and/or weakness, surgery may be a good option.
Or your surgeon may use one of a few types of spinal decompression surgery:
- Diskectomy: Removing part of a spinal disk to relieve pressure on your nerves.
- Foraminotomy: Expanding the opening for your nerve roots by removing tissue and bone.
- Laminectomy: Taking out a small portion of bone from your lower spine (lamina).
- Osteophyte removal: Removing bone spurs (osteophytes).
- Spinal fusion: During this procedure, your surgeon connects two or more vertebrae to improve stability.
Prevention
How can I prevent degenerative disk disease?
You can prevent or slow the progression of spinal degeneration through lifestyle changes. Some of these include:
- Achieving and maintaining a healthy body weight.
- Avoiding or quitting smoking.
- Exercising regularly to increase strength and flexibility.
Outlook / Prognosis
What is the outlook for people with degenerative disk disease?
Many people use nonsurgical and at-home treatments to manage pain long-term. If you have mild to moderate back pain, you will need to continue treatment to keep the pain at bay.
Most people who have surgery for degenerative disk disease experience long-term pain relief. Even after surgery, you need to continue exercising and stretching to keep your back strong and healthy.
Does degenerative disk disease increase my risk for other conditions?
Degenerated disks can increase your risk of developing other spinal conditions. Common spine problems include:
- Osteoarthritis.
- Scoliosis.
- Spinal stenosis.
- Spondylolisthesis.
- Spondylolysis.
Living With
What else should I ask my doctor?
You may want to ask your healthcare provider:
- What is the most likely cause of degenerative disk disease?
- How can I slow the progression of the disease?
- What nonsurgical treatments are most likely to relieve pain?
- What will happen if I choose not to have surgery?
- How can I prevent pain from returning after surgery?
A note from Cleveland Clinic
Degenerative disk disease occurs when your spinal disks break down. When these disks wear out, people typically experience back pain and stiffness. You may find pain relief with nonsurgical treatments such as physical therapy and spinal injection. For some people, home remedies like hot and cold therapy can decrease pain. When pain is severe, you may benefit from spinal injections or spine surgery. A spine specialist can help you determine which treatment is best for you.
Cervical Spondylosis
Cervical spondylosis is the natural wearing down of cartilage, disks, ligaments and bones in your neck. Main symptoms include neck pain or stiffness. Physical therapy; ice, heat, massage; soft collar and drugs are first-to-be-tried approaches. More severe cases, such as herniated disk, bone spurs or pinched nerves, are treated with injections or surgery.
- Appointments & Access
- Contact Us
Overview
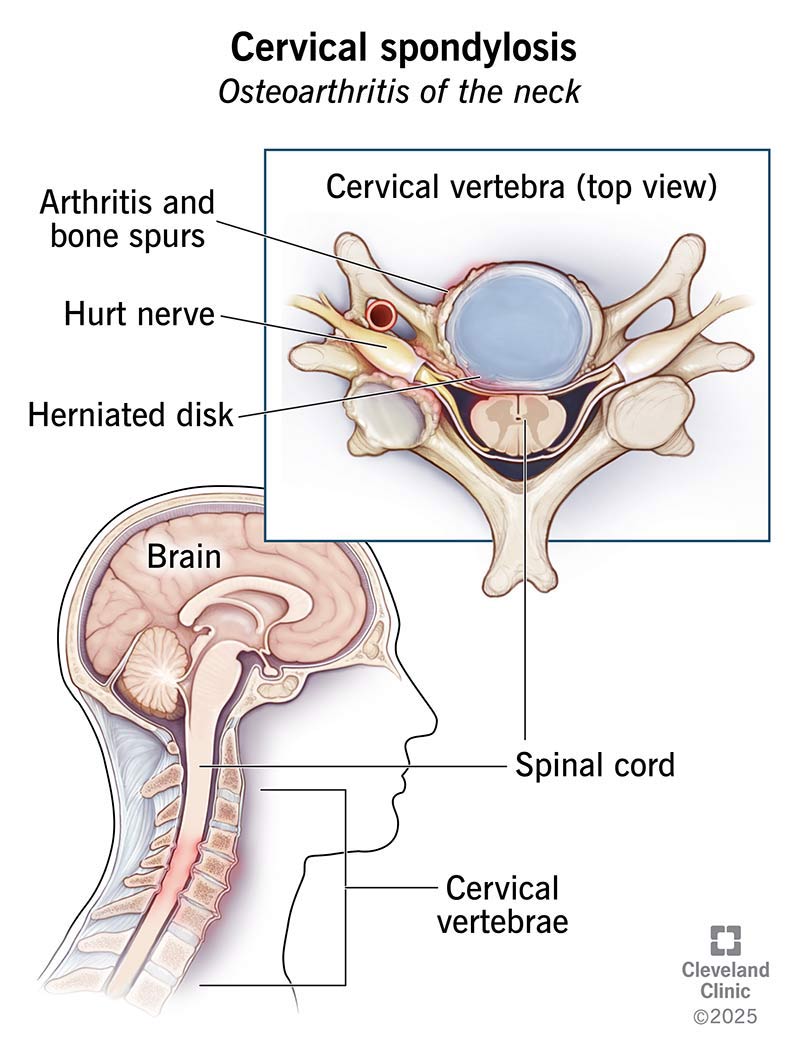
What is cervical spondylosis?
Cervical spondylosis is a general term for age-related wear and tear in the cervical spine (neck) that can lead to neck pain, neck stiffness and other symptoms. Sometimes this condition is called arthritis or osteoarthritis of the neck.
What are the parts of the cervical spine?
Your entire spine is made up of 24 vertebrae (bones of the spine). The cervical spine consists of seven vertebrae that begin at the base of the skull. Running through an opening of the entire vertebral column are the spinal cord and its nerves. The spinal cord and nerves carry messages between the brain and rest of body, including muscles and organs. Between each vertebrae are disks. The disks act like the body’s shock absorbers. The disks are made of flexible but strong connective tissue filled with a gel-like material. Disks are like “jelly-filled, cushy doughnuts” between each vertebrae.
There are three joints between each pair of vertebrae. The front joint is called the intervertebral disk. Two joints in the back of the spine are called facet joints. Within every joint is cartilage, which cushions the ends of bones. Ligaments are soft bands of tissue that connect the vertebrae together.
Spondylosis is the natural wearing down of these parts of the spine. Cartilage wears out over time, disks lose their volume and become dried and cracked, ligaments may thicken and bone spurs may form where bones rub against each other in areas that are no longer covered with cartilage. All of these changes are defined as spondylosis.
How common is cervical spondylosis?
Changes in your spine are considered a normal part of aging. The spine likely begins this wearing-down process sometime in your 30s. By age 60, almost nine in 10 people have cervical spondylosis.
Who is most at risk for getting cervical spondylosis?
Older age is a risk factor for cervical spondylosis. In addition to age, you are more likely to experience neck pain or other symptoms related to cervical spondylosis if you:
- Smoke cigarettes or used to.
- Have one or more family members with this condition.
- Strain your neck often for your job, like looking overhead (for example, painters) or downward (plumbers or flooring installers) for many hours every day or keeping your head at an improper position for long periods of time (for example, staring at a computer screen that is too high or low).
- Have a previous neck injury, such as from a car accident.
- Do heavy lifting like construction workers.
- Are exposed to a lot of vibration like bus or truck drivers.
Symptoms and Causes
What causes cervical spondylosis?
As you get older, your spine undergoes changes due to decades of normal wear and tear. Starting in middle age, the disks between your vertebrae start to change. These changes can include:
- Degeneration: The spinal disks in your neck may slowly wear down (degenerate). With time, the disks become thinner, and the soft tissue has less elasticity. If you or your parents measure in a little shorter in height than you did years ago, this is normal collapsing or settling of your disks.
- Herniation: Normal aging can cause part of your spinal disk to tear or crack. This is called a herniated disk. The herniation can allow the disk to bulge out, pressing on nearby tissue or a spinal nerve. This pressure can cause pain, tingling or numbness.
- Osteoarthritis: Osteoarthritis is a progressive (ongoing) condition that causes cartilage in your joints to degenerate (wear down with time). With osteoarthritis, cartilage degenerates faster than with normal aging.
- Bone spurs: When cartilage in the joints of the vertebrae in your spine starts to degenerate and bone tissue rubs directly against other bone tissue, abnormal bone growths develop along the edges of vertebrae. These growths (called osteophytes or bone spurs) are common as you age. Often, they cause no symptoms.
What are the most common cervical spondylosis symptoms?
You may have cervical spondylosis and not even know it. It’s common to have no symptoms related to this condition.
If you do experience symptoms, symptoms typically include:
- Neck pain or stiffness. This may be the main symptom. Pain may get worse when you move your neck.
- A nagging soreness in the neck.
- Muscle spasms.
- A clicking, popping or grinding sound when you move your neck.
- Dizziness.
- Headaches.
What is cervical myelopathy?
As your vertebral disks wear away with time, your spinal cord can be put under increased pressure as the canal gets narrower from arthritis and disk protrusions. This compression can result in worsening neck pain and other symptoms. This condition is called cervical spondylotic myelopathy (CSM).
If you have CSM, you have the symptoms seen with cervical spondylosis, plus these additional symptoms:
- Weakness, tingling or numbness in one or both arms or legs.
- Loss of bladder and bowel control.
- Trouble walking (feeling unsteady on your feet).
- Loss of function in hands, like having problems writing.
Symptoms related to CSM may slowly get worse over time. If your symptoms don’t go away, or if they significantly affect your life, your healthcare provider may refer you to a spine surgeon who specializes in treating this condition.
Diagnosis and Tests
How do healthcare providers diagnose cervical spondylosis?
Your healthcare provider will perform a physical exam to find the cause of your neck pain or other symptoms.
Your symptoms and their severity give clues to how much pressure your cervical spine might be under. During a physical exam, your healthcare provider may check your:
- Neck flexibility.
- Muscle strength and reflexes in your hands, arms or legs.
- Reflexes.
- Gait (how you walk).
- Neck and shoulder, looking for trigger points (a small bump or knot in the muscle of your neck or shoulder that may be the source of your pain and tenderness).
Sometimes, healthcare providers can diagnose cervical spondylosis with just a physical exam. Other times, they may order tests to learn more about what may be causing your symptoms. These tests may include the following:
- X-rays show the bones in your neck, their alignment, loss of bone and bone spurs (if present). Not all bone changes cause symptoms. Healthcare providers may use X-rays as a starting point. X-rays or other tests can also help rule out other causes of your discomfort, such as a spine tumor.
- Computed tomography (CT) scans provide more detail than X-rays. This scan can help better view the spinal canal and bone spurs.
- MRIimages show the details of soft tissues such as cartilage, nerve roots, muscles, spinal cord and disks. This test can show spinal compression or herniated disk more clearly than X-rays.electromyelography An MRI can help identify the source and location of pain.
- Other tests may include a myelogram(type of CT scan) or electromyogram (nerve function test). These tests provide more details on how cervical spondylosis may be affecting your nerves.
Management and Treatment
What are common cervical spondylosis treatments?
Cervical spondylosis does not always cause symptoms. Without symptoms, you may not need treatment at all.
When your condition does cause symptoms, conservative treatments effectively treat most cases. Your healthcare provider may recommend:
- Physical therapy: Your symptoms may be relieved with specific exercises and stretches. Physical therapy focuses on stretching and strengthening your muscles and improving your posture. You may do these stretches at home or need the assistance of a physical therapist at a clinic. Your healthcare provider will advise how long and how often you should practice these exercises, based on your individual symptoms and condition.
- Ice, heat and massage can help relieve your symptoms. You’ll have to conduct your own trial to see if heat or cold best relieve your pain and discomfort. Apply heat or ice typically no more than 20 minutes at a time, several times a day. Massage is another option that may be tried in some patients. Ask your healthcare provide if this is a reasonable option for what’s causing your specific problem.
- Oral medications: Depending on how much pain you’re in, a healthcare provider might recommend prescription or over-the-counter anti-inflammatory drugs like ibuprofen (Advil®, Motrin®) or naproxen sodium (Aleve®). Muscle relaxants such as cyclobenzaprine (Amrix®, Fexmid®) can treat muscle spasms. For severe arm pain from nerve impingement, gabapentin (Neurontin®) may reduce the pain.
- Soft collar or brace: Your healthcare provider may recommend you wear a therapeutic collar for a short time. This can limit neck movement and help strained muscles rest and recuperate. Wearing a brace for too long can lead to muscle atrophy (wasting away). Only use a collar under the guidance of a medical professional.
- Injection therapy: Steroids can be injected into the affected area of the spine. Injection medications can make your symptoms better for a short period of time. There are three common steroid injection procedures:
- Cervical epidural block: Neck or arm pain due to cervical disk herniation can be treated with an injection of a combination of a steroid and anesthetic. The injection is made into the epidural space, which is the space next to the covering of the spinal cord.
- Cervical facet joint block: This steroid plus anesthetic injection is made into small joints at the affected segments of the cervical spine.
- Media branch block and radiofrequency ablation: This technique is used to both diagnosis and treat chronic neck pain. If pain is relieved with an injection of an anesthetic, that spot is identified for treatment. The treatment, called radiofrequency ablation, involves damaging the nerves with sound waves that are causing pain in the joint.
For the most severe cases of cervical spondylosis – including cervical myelopathy or cervical radiculopathy – your healthcare providers may consider surgery. Surgeries can involve removing bone spurs and fusing together the vertebrae or creating more room for the spinal cord by removing a portion of vertebrae.
Spine surgery is complex and may involve a lengthy recovery. Your healthcare provider will consider your symptoms, condition and overall health before deciding whether surgery may benefit you.
Prevention
Are there ways to prevent cervical spondylosis from occurring?
There is no way to prevent cervical spondylosis as this condition is a normal, age-related deterioration (“wear and tear”) of the joint space and disks in your neck.
If you do have a job or a hobby that results in a lot of time spent looking overhead, downward or having your head in an awkward posture, take many short breaks in your day (if possible). Learn proper stretching and strengthening exercises from your healthcare provider or physical therapist.
Follow other self-help therapies such as applying ice or heat to your neck to ease muscle soreness and pain and taking over-the-counter anti-inflammatory drugs and pain-killers such as ibuprofen or naproxen.
Always follow the instructions of your healthcare professionals and physical therapist.
Outlook / Prognosis
What can I expect if I think I have (or have a diagnosis of) cervical spondylosis?
At first, you may not even have any symptoms. However, since cervical spondylosis is an age-related degenerative condition, if you are in your 60s, 70s, 80s or older you may have such symptoms as neck pain and stiffness to start. If you are young, you can still develop this condition if you have jobs or hobbies that cause your head and neck to be out of good alignment for long periods of time. Fortunately, most early symptoms of pain and discomfort can be treated with simple at-home and over-the-counter remedies.
Some people may go on to develop more complicated issues such as disk herniation, bone spurs, pinched nerves and nerve compression. These conditions may require an increasing amount of medical care, ranging range prescription medications, to steroid injections to surgery.
When should I call the healthcare provider?
Most cases of neck pain go away on their own or with nonsurgical treatments. If neck pain or discomfort lasts more than a few days, reach out to your healthcare provider for guidance.
Seek immediate medical care if you have:
- Severe pain or pain that is worsening.
- Numbness or tingling in arms.
- Trouble with coordination, trouble walking.
- Muscle weakness or heaviness in arms or legs.
- Loss of bladder or bowel control.
Living With
What the difference between cervical spondylosis and spondylitis, spondylolysis and spondylolisthesis?
Cervical spondylosis is a degeneration – or breakdown – of the spine and disks in your neck. It is a general term for the situation that occurs in your neck area. It is an arthritis of the joints (the spaces) between the vertebrae in the neck.
Spondylitis is inflammation of one or more vertebrae. “Itis” means inflammation. Ankylosing spondylitis is a type of arthritis in your spine. Ankylosing spondylitis can result in vertebrae fusing together.
Spondylolysis is a physical break in the mid-arch area of a section of vertebrae called the pars interarticularis. The pars interarticularis are the horizontal pieces on the sides of the main body of each vertebrae – the “wings” on the body of each vertebrae. This condition is usually caused by injury, trauma or overuse by hyperextension (for example, weight lifters, tennis players). Spondylolysis usually occurs in the lumber (lower back) spine.
Cervical spondylolisthesis is a specific condition in which one vertebra slips forward over the vertebrae beneath it. A fracture (break) or injury of the vertebrae of the spine can cause the vertebra to start to shift out of place.
What is radiculopathy?
Radiculopathy is a pinching of a nerve at the nerve root. The nerve root is the first segment of nerve as it branches off of the spinal cord within the spinal column.